Key Takeaways
- Alzheimer’s disease is a progressive neurodegenerative disorder affecting memory, thinking, and behavior.
- Oxidative stress, including from excess iron, plays a significant role in Alzheimer’s progression.
- Managing Alzheimer’s involves addressing mineral imbalances, optimizing diet, and avoiding ultra-processed foods.
- Current treatments focus on symptom management, with ongoing research into disease-modifying therapies.
- Support systems for patients and caregivers are essential for quality of life.
Introduction to Alzheimer’s Disease
Alzheimer’s disease is a neurodegenerative disorder characterized by the gradual loss of memory, cognitive function, and behavioral changes.
It is the most common cause of dementia, affecting millions of people worldwide.
As the disease progresses, it profoundly impacts the individual’s ability to perform daily tasks, leading to increased dependence on caregivers.
Causes and Risk Factors
Genetic Factors:
Alzheimer’s disease has a strong genetic component, with the APOE-e4 gene being one of the most significant risk factors.
Individuals with one or more copies of this gene are at a higher risk of developing the disease, especially at an earlier age.

Environmental and Lifestyle Factors:
Lifestyle choices, including diet, exercise, and exposure to toxins, can influence the risk of developing Alzheimer’s.
For example, a diet high in ultra-processed foods and excessive carbohydrates may increase the risk, while a diet rich in whole foods close to ancestral eating patterns can be protective.
Age and Gender:
The risk of Alzheimer’s increases with age, particularly after age 65. Women are more likely to develop Alzheimer’s than men, partly due to longer life expectancy.
Iron’s Role in Alzheimer’s:
Excess iron contributes to oxidative stress, a key factor in the development and progression of Alzheimer’s.
The accumulation of iron in the brain can lead to neuronal damage, increasing the risk of Alzheimer’s.
Oxidative Stress in Alzheimer’s Disease
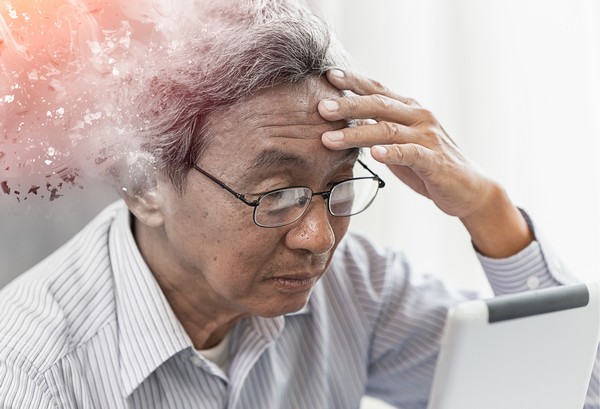
Oxidative Stress and Neuronal Damage:
Oxidative stress occurs when there is an imbalance between free radicals and antioxidants in the body.
In Alzheimer’s, oxidative stress leads to the degeneration of neurons, contributing to cognitive decline and memory loss.
Iron and the Fenton Reaction:
Excess iron in the brain can catalyze the production of reactive oxygen species (ROS) through the Fenton reaction.
These ROS cause significant damage to brain cells, accelerating the progression of Alzheimer’s.
Importance of Mineral Balance:
Maintaining a balance of essential minerals, particularly ensuring optimal levels of bioavailable copper and magnesium, is crucial in mitigating oxidative stress.
These minerals play a protective role by supporting healthy brain function and reducing the harmful effects of excess iron.
Inflammation and Iron Accumulation:
Chronic inflammation can lead to increased iron accumulation in the brain, exacerbating oxidative stress.
This creates a vicious cycle of inflammation and neuronal damage that accelerates Alzheimer’s progression.
Brain Changes in Alzheimer’s Disease
Amyloid Plaques and Tau Tangles:
The hallmark features of Alzheimer’s disease include the buildup of amyloid plaques and tau tangles in the brain.
These abnormal protein deposits disrupt communication between brain cells, leading to their eventual death and contributing to the symptoms of Alzheimer’s.
Neurotransmitter Imbalances:
Oxidative stress and mineral imbalances, particularly related to iron and copper, can disrupt neurotransmitter systems in the brain.
A key example is the decline in acetylcholine, a neurotransmitter critical for memory and learning, which is particularly affected in Alzheimer’s patients.
Diagnosis of Alzheimer’s Disease

Early Signs and When to See a Doctor:
Early symptoms of Alzheimer’s include memory loss, difficulty in planning or solving problems, confusion about time or place, and changes in mood or personality.
It’s important to consult a healthcare professional if these symptoms are noticed, as early diagnosis can help in managing the disease more effectively.
Diagnostic Tools and Tests:
Alzheimer’s is diagnosed using a combination of cognitive tests, brain imaging techniques like MRI and PET scans, and biomarkers such as beta-amyloid and tau levels in cerebrospinal fluid.
Comprehensive blood tests may also be used to assess mineral imbalances that could be contributing to the disease.
Importance of Early Diagnosis:
Early diagnosis allows for better management of symptoms and planning for the future. It also provides an opportunity to start treatments that may slow the disease’s progression.
Current Treatments and Management Strategies
Medications for Symptom Management:
Currently, several FDA-approved medications help manage the symptoms of Alzheimer’s by improving neurotransmitter function.
These include cholinesterase inhibitors and memantine, which can help with memory and cognitive function.
Addressing Oxidative Stress and Iron Regulation:
To manage oxidative stress, treatments may include antioxidants, such as vitamin E.
Lactoferrin, found in colostrum, helps regulate iron levels, making it a beneficial supplement for those with high iron levels.
Ensuring optimal levels of bioavailable copper and magnesium is also important in maintaining brain health.
Non-Pharmacological Interventions:
Cognitive therapy, physical activity, and other lifestyle changes play a significant role in managing Alzheimer’s symptoms.
Regular exercise, mental stimulation, and maintaining a routine can help slow cognitive decline and improve quality of life.
Emerging Therapies and Research:
Research into Alzheimer’s is ongoing, with new therapies focusing on disease-modifying treatments that target the underlying causes, such as oxidative stress and amyloid plaque formation.
Gene therapy, immunotherapy, and precision medicine are promising areas of study.
Lifestyle and Prevention
Diet and Nutrition:
A diet rich in whole foods that are close to ancestral diets can help reduce Alzheimer’s risk.
Avoiding ultra-processed foods, excess carbohydrates, and foods artificially fortified with iron is important.
Emphasizing nutrient-dense foods that support optimal mineral balance, such as seafood and grass-fed meat, is recommended.
Physical Activity:
Regular exercise is beneficial for brain health and may help delay the onset of Alzheimer’s.
Physical activity improves blood flow to the brain, supports cardiovascular health, and reduces inflammation, all of which contribute to maintaining cognitive function.
Cognitive Engagement:
Mental stimulation through activities like reading, puzzles, and social interaction is important for brain health.
Keeping the mind active helps build cognitive reserve, which can delay the onset of Alzheimer’s symptoms.
Sleep and Stress Management:
Quality sleep and stress reduction are important for brain health. Poor sleep and chronic stress increase the risk of Alzheimer’s by contributing to inflammation and oxidative stress.
Practicing good sleep hygiene and stress management techniques, such as mindfulness and meditation, can support cognitive health.
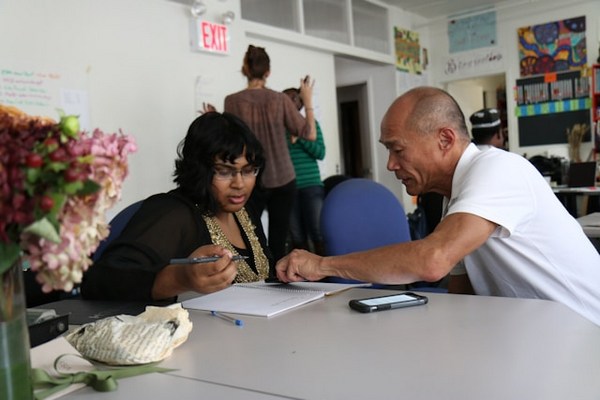
Support for Patients and Caregivers
Coping Strategies for Patients:
Living with Alzheimer’s requires coping strategies to manage daily challenges. Using memory aids, maintaining a routine, and creating a safe home environment can help patients maintain independence for as long as possible.
Caregiver Support and Resources:
Caregivers face significant challenges and require support to manage the demands of caregiving.
Resources such as support groups, respite care, and counseling can help caregivers maintain their well-being while providing care for their loved ones.
Legal and Financial Planning:
Early planning for legal and financial matters is essential as Alzheimer’s progresses. This includes setting up power of attorney, creating a living will, and planning for long-term care.
Consulting with professionals who specialize in elder law and financial planning can help ensure that the patient’s wishes are respected and that their needs are met.
The Future of Alzheimer’s Research

Promising Areas of Research:
Research into Alzheimer’s is expanding, with promising studies focused on understanding the role of iron metabolism, oxidative stress, and the development of new therapies.
Advances in genetic research, biomarkers, and early detection methods are also paving the way for more effective treatments.
The Role of Clinical Trials:
Clinical trials are essential for developing new treatments and finding a cure for Alzheimer’s. Patients and families can participate in trials to contribute to research efforts and potentially gain access to cutting-edge treatments.
Public Health Initiatives and Awareness:
Raising awareness about Alzheimer’s and its risk factors is crucial for public health. Initiatives aimed at educating the public, supporting research, and advocating for policies that address the needs of Alzheimer’s patients and caregivers are essential in the fight against this disease.
Iron Metabolism and Neurodegeneration:
- A significant number of studies investigate the role of iron in neurodegenerative diseases. This includes the examination of brain iron metabolism (e.g., Ke & Qian, 2007; Yuan et al., 2023), iron overload and its effects on cognitive function (e.g., Wang et al., 2018), and the mechanisms of iron transport and homeostasis in the brain (e.g., Moos et al., 2007; Mills et al., 2009).
Cognitive Impairment and Alzheimer’s Disease:
- Research explores various aspects of cognitive decline, particularly Alzheimer’s disease. This includes the amyloid cascade hypothesis (Hardy & Higgins, 1992), the impact of glucose metabolism and ketone bodies on cognitive function (e.g., Krikorian et al., 2012; Hertz et al., 2015), and the vascular contributions to cognitive impairment and dementia (e.g., Gorelick et al., 2011).
Mechanisms and Pathophysiology:
- Several articles focus on the mechanisms underlying neurodegeneration, such as the effects of glucose hypometabolism (Daulatzai, 2016), and the interactions between brain iron metabolism and other neurobiological processes (e.g., Rouault, 2013; Sweeney et al., 2016).
Clinical and Experimental Insights:
- Some studies offer insights into experimental models and clinical implications, including the role of selective iron chelation in conditions like Friedreich ataxia (Boddaert et al., 2007) and the potential therapeutic approaches for neurodegenerative diseases (e.g., Vanlandingham et al., 2023).
Frequently Asked Questions (FAQ)
What are the early signs of Alzheimer’s?
Early signs include memory loss, confusion, difficulty in planning, and changes in mood or personality.
Can Alzheimer’s be prevented?
While there is no guaranteed way to prevent Alzheimer’s, maintaining a healthy lifestyle with a balanced diet, regular exercise, and mental stimulation can reduce the risk.
How does oxidative stress contribute to Alzheimer’s?
Oxidative stress damages brain cells by producing harmful free radicals, which can accelerate the progression of Alzheimer’s.
What role does iron play in the development of Alzheimer’s?
Excess iron can contribute to oxidative stress, leading to neuronal damage and increasing the risk of Alzheimer’s. Regulating iron levels with lactoferrin from colostrum and ensuring a balance of essential minerals can help mitigate this risk.
How can diet and lifestyle changes help prevent or manage Alzheimer’s?
A diet rich in whole, nutrient-dense foods, regular physical activity, mental engagement, and good sleep hygiene can help prevent or manage Alzheimer’s by supporting brain health and reducing oxidative stress.
What are the benefits of colostrum and lactoferrin in managing iron levels?
Colostrum contains lactoferrin, a protein that helps regulate iron levels in the body, reducing the risk of iron-induced oxidative stress and supporting overall brain health.
Research
Batey RG, Lai Chung Fong P, Shamir S, Sherlock S. A non-transferrin-bound serum iron in idiopathic hemochromatosis. Dig Dis Sci. 1980 May;25(5):340-6. doi: 10.1007/BF01308057. PMID: 7371472.
Bateman RJ, Aisen PS, De Strooper B, et al. Autosomal-dominant Alzheimer’s disease: A review and proposal for the prevention of Alzheimer’s disease. Alzheimers Res Ther 2011;3(1):1. doi: 10.1186/alzrt59.
Bermejo‐Pareja, F., del Ser, T., Valentí, M., de la Fuente, M., Bartolome, F. and Carro, E., 2020. Salivary lactoferrin as biomarker for Alzheimer’s disease: Brain‐immunity interactions. Alzheimer’s & Dementia, [online] 16(8), pp.1196–1204. https://doi.org/10.1002/alz.12107.
Boddaert, N., Le Quan Sang, K. H., Rötig, A., Leroy-Willig, A., Gallet, S., Brunelle, F., Sidi, D., Thalabard, J., Munnich, A., & Cabantchik, Z. I. (2007). Selective iron chelation in Friedreich ataxia: Biologic and clinical implications. Blood, 110(1), 401-408. https://doi.org/10.1182/blood-2006-12-065433
Carro, E., Bartolomé, F., Bermejo-Pareja, F., Villarejo-Galende, A., Molina, J. A., Ortiz, P., Calero, M., Rabano, A., Cantero, J. L., & Orive, G. (2017). Early diagnosis of mild cognitive impairment and Alzheimer's disease based on salivary lactoferrin. Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring, 8, 131-138. https://doi.org/10.1016/j.dadm.2017.04.002
Crane, P.K., Walker, R., Hubbard, R.A., Li, G., Nathan, D.M., Zheng, H., Haneuse, S., Craft, S., Montine, T.J., Kahn, S.E., McCormick, W., McCurry, S.M., Bowen, J.D. and Larson, E.B., 2013. Glucose Levels and Risk of Dementia. New England Journal of Medicine, [online] 369(6), pp.540–548. https://doi.org/10.1056/nejmoa1215740.
Cunnane, S.C., Courchesne‐Loyer, A., St‐Pierre, V., Vandenberghe, C., Pierotti, T., Fortier, M., Croteau, E. and Castellano, C., 2016. Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer’s disease. Annals of the New York Academy of Sciences, [online] 1367(1), pp.12–20. https://doi.org/10.1111/nyas.12999.
Daulatzai, M.A., 2016. Cerebral hypoperfusion and glucose hypometabolism: Key pathophysiological modulators promote neurodegeneration, cognitive impairment, and Alzheimer’s disease. Journal of Neuroscience Research, [online] 95(4), pp.943–972. https://doi.org/10.1002/jnr.23777.
DiNicolantonio, J.J., Mangan, D. and O’Keefe, J.H., 2018. The fructose–copper connection: Added sugars induce fatty liver and insulin resistance via copper deficiency. Journal of Metabolic Health, [online] 3(1).
https://doi.org/10.4102/jir.v3i1.43.
Duyn, J.H., 2010. Study of brain anatomy with high-field MRI: recent progress. Magnetic Resonance Imaging, [online] 28(8), pp.1210–1215. https://doi.org/10.1016/j.mri.2010.02.007.
Fillebeen, C., Descamps, L., Dehouck, M.-P., Fenart, L., Benaïssa, M., Spik, G., Cecchelli, R. and Pierce, A., 1999. Receptor-mediated Transcytosis of Lactoferrin through the Blood-Brain Barrier. Journal of Biological Chemistry, [online] 274(11), pp.7011–7017. https://doi.org/10.1074/jbc.274.11.7011.
Garrett, L. R., & Niccoli, T. (2022). Frontotemporal Dementia and Glucose Metabolism. Frontiers in Neuroscience, 16, 812222. https://doi.org/10.3389/fnins.2022.812222
Galaris, D., Barbouti, A. and Pantopoulos, K., 2019. Iron homeostasis and oxidative stress: An intimate relationship. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research, [online] 1866(12), p.118535. https://doi.org/10.1016/j.bbamcr.2019.118535.
Gorelick, P.B., Scuteri, A., Black, S.E., DeCarli, C., Greenberg, S.M., Iadecola, C., Launer, L.J., Laurent, S., Lopez, O.L., Nyenhuis, D., Petersen, R.C., Schneider, J.A., Tzourio, C., Arnett, D.K., Bennett, D.A., Chui, H.C., Higashida, R.T., Lindquist, R., Nilsson, P.M., Roman, G.C., Sellke, F.W. and Seshadri, S., 2011. Vascular Contributions to Cognitive Impairment and Dementia. Stroke, [online] 42(9), pp.2672–2713. https://doi.org/10.1161/str.0b013e3182299496.
Gutteridge, J.M.C. and Halliwell, B., 2018. Mini-Review: Oxidative stress, redox stress or redox success? Biochemical and Biophysical Research Communications, [online] 502(2), pp.183–186.
https://doi.org/10.1016/j.bbrc.2018.05.045.
Hardy JA, Higgins GA. Alzheimer’s disease: The amyloid cascade hypothesis. Science 1992;256(5054):184–85. doi: 10.1126/science.1566067.
Hentz, M.W., Muckenthaler, M.U., Galy, B. and Camaschella, C., 2010. Two to Tango: Regulation of Mammalian Iron Metabolism. Cell, [online] 142(1), pp.24–38. https://doi.org/10.1016/j.cell.2010.06.028.
Hertz, L., Chen, Y. and Waagepetersen, H.S., 2015. Effects of ketone bodies in Alzheimer’s disease in relation to neural hypometabolism, β‐amyloid toxicity, and astrocyte function. Journal of Neurochemistry, [online] 134(1), pp.7–20. https://doi.org/10.1111/jnc.13107.
Kenkhuis, B., Bush, A.I. and Ayton, S., 2023. How iron can drive neurodegeneration. Trends in Neurosciences, [online] 46(5), pp.333–335.
https://doi.org/10.1016/j.tins.2023.02.003.
Ke, Y. and Qian, Z.M., 2007. Brain iron metabolism: Neurobiology and neurochemistry. Progress in Neurobiology, [online] 83(3), pp.149–173. https://doi.org/10.1016/j.pneurobio.2007.07.009.
Krikorian, R., Shidler, M. D., Dangelo, K., Couch, S. C., Benoit, S. C., & Clegg, D. J. (2012). Dietary ketosis enhances memory in mild cognitive impairment. Neurobiology of Aging, 33(2), 425.e19. https://doi.org/10.1016/j.neurobiolaging.2010.10.006
Kruszewski, M., 2003. Labile iron pool: the main determinant of cellular response to oxidative stress. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis, [online] 531(1–2), pp.81–92.
https://doi.org/10.1016/j.mrfmmm.2003.08.004.
Lane CA, Hardy J, Schott JM. Alzheimer’s disease. Eur J Neurol 2018;25(1):59–70. doi: 10.1111/ene.13439.
Mason, S. T., & Fibiger, H. C. (1979). Regional topography within noradrenergic locus coeruleus as revealed by retrograde transport of horseradish peroxidase. Journal of Comparative Neurology, 187(4), 703-724. https://doi.org/10.1002/cne.901870405
Mills, E., Dong, X., Wang, F. and Xu, H., 2009. Mechanisms of Brain Iron Transport: Insight into Neurodegeneration and CNS Disorders. Future Medicinal Chemistry, [online] 2(1), pp.51–64. https://doi.org/10.4155/fmc.09.140.
Mohamed, W. A., Salama, R. M., & Schaalan, M. F. (2019). A pilot study on the effect of lactoferrin on Alzheimer’s disease pathological sequelae: Impact of the p-Akt/PTEN pathway. Biomedicine & Pharmacotherapy, 111, 714-723. https://doi.org/10.1016/j.biopha.2018.12.118
Moos, T., Nielsen, T.R., Skjørringe, T. and Morgan, E.H., 2007. Iron trafficking inside the brain. Journal of Neurochemistry, [online] 103(5), pp.1730–1740. https://doi.org/10.1111/j.1471-4159.2007.04976.x.
Moos, T, Morgan EH. Transferrin and transferrin receptor function in brain barrier systems. Cell Mol Neurobiol. 2000 Feb;20(1):77-95. doi: 10.1023/a:1006948027674. PMID: 10690503.
Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197-213. doi: 10.1146/annurev.nutr.28.061807.155521. PMID: 18489257.
Petok, J.R., Merenstein, J.L. and Bennett, I.J., 2024. Iron content affects age group differences in associative learning-related fMRI activity. NeuroImage, [online] 285, p.120478. https://doi.org/10.1016/j.neuroimage.2023.120478.
Rawlings, A.M., Sharrett, A.R., Mosley, T.H., Ballew, S.H., Deal, J.A. and Selvin, E., 2017. Glucose Peaks and the Risk of Dementia and 20-Year Cognitive Decline. Diabetes Care, [online] 40(7), pp.879–886. https://doi.org/10.2337/dc16-2203.
Rouault, T. A. (2013). Iron metabolism in the CNS: implications for neurodegenerative diseases. Nat Rev Neurosci 14, 551–564. https://doi.org/10.1038/nrn3561
Sweeney MD, Ayyadurai S, Zlokovic BV. Pericytes of the neurovascular unit: Key functions and signaling pathways. Nat Neurosci. 2016 Jun;19(6):771-83. doi: 10.1038/nn.4295. Epub 2016 May 23. PMID: 27214663; PMCID: PMC4902634.
Sweeney MD, Sagare AP, Zlokovic BV. Blood–brain barrier breakdown in Alzheimer’s disease and other neurodegenerative disorders. Nat Rev Neurol. 2018 Nov;14(11):133-150. doi: 10.1038/s41582-018-0007-8. Epub 2018 Sep 21. PMID: 30250470; PMCID: PMC6202551.
Van Houten, B., 2020. Mitochondrial Dysfunction and Iron: A Dangerous Liaison. Cell Metabolism, 31(5), 785–786. https://doi.org/10.1016/j.cmet.2020.04.007.
Vanlandingham, J., Grinberg, I., McMillan, P., Jones, L. A., & Bostwick, C. (2023). Investigating brain iron metabolism: new approaches and advances. Frontiers in Neuroscience, 17, 105192. https://doi.org/10.3389/fnins.2023.105192
Wang, X., Zhang, Z., Wang, Y., Zheng, Z., & Xu, H. (2018). Iron overload and cognitive impairment: insights from rodent and human studies. Current Alzheimer Research, 15(4), 350-361. https://doi.org/10.2174/15672050156661802061526
Ward, R.J., Zucca, F.A., Duyn, J.H., Crichton, R.R. and Zecca, L., 2014. The role of iron in brain ageing and neurodegenerative disorders. The Lancet Neurology, [online] 13(10), pp.1045–1060.
https://doi.org/10.1016/s1474-4422(14)70117-6.
Yuan, J., Zhang, J., Xu, M., & Liu, Y. (2023). Role of iron metabolism in neurodegenerative diseases: A review. Frontiers in Aging Neuroscience, 15, 740912. https://doi.org/10.3389/fnagi.2023.740912
Mental Benefits of Learning a New Language
Key Takeaways: Enhances brain volume and memory. Improves cognitive flexibility, multitasking, and executive functions. Delays cognitive decline and boosts emotional intelligence. Increases empathy, cultural awareness,…
Anxiety: Causes, Symptoms, and Management
Key Takeaways: Anxiety can disrupt daily life when it becomes overwhelming. Common symptoms include restlessness, rapid heartbeat, and difficulty concentrating. Causes include stress, genetics, and…
Supporting Mental Health with Gut Health
Key Takeaways Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis. Probiotics: Beneficial bacteria that help regulate mood and support…
Parkinson’s Disease : Symptoms, Causes & Treatment
Key Takeaways Parkinson’s disease is a progressive neurological disorder that affects movement and coordination. Oxidative stress and excess iron are significant factors in the progression…
Reduce Stress through Pet Therapy
Key Highlights Pet therapy, or animal-assisted therapy, boosts health. Interacting with animals lowers cortisol, blood pressure, and heart rate. Therapy, service, and companion animals are…
Dementia: Causes, Symptoms, and Management
Key Takeaways: Dementia involves a decline in cognitive function affecting memory, thinking, and daily life. Common causes include genetic factors, aging, and certain medical conditions….
GABA (gamma-aminobutyric acid)
Key Takeaways GABA is a neurotransmitter that helps calm the nervous system. Low GABA levels can lead to anxiety, stress, and sleep problems. Natural precursors…
Say Goodbye to Depression with Natural Remedies
Key Takeaways Regular exercise, sufficient sleep, and a diet full of bioavailable nutrients support mental health. Spending time in nature, like forest bathing and gardening,…
Mastering Emotional Healing: Your Guide to Recovery
Key Highlights Emotional healing is a gradual process requiring patience and self-compassion. Acknowledge and accept your feelings, and identify sources of emotional pain. Embrace vulnerability,…
Fight, Flight, Freeze, Fawn: Stress Response Examined
Key Takeaways The stress response includes four primary reactions, each serving as a survival mechanism. The fight response involves confronting the threat, often with aggression…
Emotional Freedom Technique (EFT): Tap to relieve stress
Key Highlights Learn about the origins and principles of Emotional Freedom Technique (EFT) for stress relief. Understand the science-backed mechanisms of how EFT works on…