Key Takeaways:
- Dementia involves a decline in cognitive function affecting memory, thinking, and daily life.
- Common causes include genetic factors, aging, and certain medical conditions.
- Early symptoms often involve memory loss, mood changes, and difficulty with communication.
- Management includes medication, lifestyle adjustments, and caregiver support.
- Preventive measures focus on healthy living and managing chronic diseases.
Introduction to Dementia
Dementia refers to a group of conditions marked by a decline in cognitive abilities severe enough to interfere with daily activities.
Alzheimer’s disease is the most common type, but other forms include vascular dementia, Lewy body dementia, and frontotemporal dementia.
Causes and Risk Factors
Dementia can arise from several causes, with age being the most significant factor. Genetics also contribute, particularly in early-onset cases.
Medical conditions like hypertension, diabetes, and cardiovascular disease increase the risk, as do lifestyle factors such as smoking, poor diet, and lack of exercise.
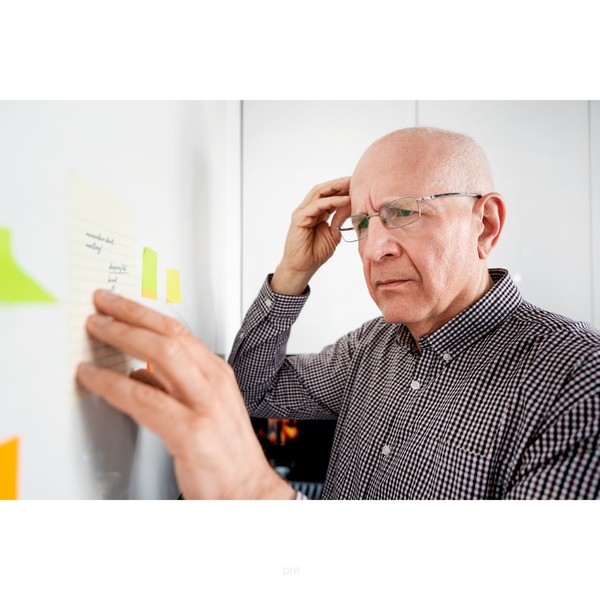
Symptoms and Early Signs

Dementia symptoms vary, but common early signs include memory loss, especially of recent events.
Individuals may experience confusion, have trouble with language, and struggle with problem-solving. Mood changes, including depression, anxiety, and irritability, often accompany cognitive decline.
These symptoms progressively impair the ability to perform everyday tasks.
Diagnosis of Dementia
Diagnosing dementia requires a comprehensive medical evaluation. Doctors typically conduct cognitive tests to assess memory, language, and problem-solving abilities.
Brain imaging, such as MRI or CT scans, helps detect changes in brain structure. Blood tests and other assessments are used to rule out other possible causes of symptoms.
Treatment and Management

While there is no cure for dementia, treatments aim to manage symptoms and improve quality of life.
Lifestyle changes, including a balanced diet and regular physical activity, support overall brain health. When done properly, the ketogenic diet in particular can provide significant benefits on multiple fronts.
Caregiver support is essential, providing emotional and practical assistance to those affected.
Medications like cholinesterase inhibitors and memantine can help manage cognitive symptoms.
Coping with Dementia
Living with dementia requires adapting to new challenges. Establishing routines and using memory aids can help maintain independence.
Strong support networks, including family, friends, and professional caregivers, are vital. Legal and financial planning ensures future needs are met.
Prevention and Risk Reduction
Preventing dementia involves adopting healthy lifestyle habits.
Regular exercise, a diet rich in nutrients, and mental stimulation are key strategies.
Social engagement also supports cognitive health. Managing chronic conditions like hypertension and diabetes can reduce the risk of developing dementia.
FAQ
What is dementia?
Dementia is a condition marked by a decline in cognitive function, affecting memory, thinking, and daily activities.
What causes dementia?
Dementia can be caused by genetic factors, aging, medical conditions like hypertension and diabetes, and lifestyle choices.
How is dementia diagnosed?
Diagnosis involves cognitive tests, brain imaging, and medical evaluations to assess symptoms and rule out other conditions.
Can dementia be treated?
While dementia cannot be cured, treatments focus on managing symptoms, improving quality of life, and providing caregiver support.
What can be done to prevent dementia?
Prevention involves maintaining a healthy lifestyle, including regular exercise, a nutrient-rich diet, and mental and social engagement.
Research
Abbasi, U., Abbina, S., Gill, A., Takuechi, L.E., & Kizhakkedathu, J.N. (2021). Role of Iron in the Molecular Pathogenesis of Diseases and Therapeutic Opportunities. ACS Chemical Biology, 16(6), 945–972. https://doi.org/10.1021/acschembio.1c00122
Atkins, J.L., Pilling, L.C., Heales, C.J., Savage, S., Kuo, C.-L., Kuchel, G.A., Steffens, D.C., & Melzer, D. (2021). Hemochromatosis Mutations, Brain Iron Imaging, and Dementia in the UK Biobank Cohort. Journal of Alzheimer’s Disease, 79(3), 1203–1211. https://doi.org/10.3233/jad-201080
Bader, V., & Winklhofer, K.F. (2020). Mitochondria at the Interface between Neurodegeneration and Neuroinflammation. Seminars in Cell & Developmental Biology, 99, 163–171.
Bellou V, Belbasis L, Tzoulaki I, Middleton LT, Ioannidis JPA, Evangelou E. Systematic evaluation of the associations between environmental risk factors and dementia: An umbrella review of systematic reviews and meta-analyses. Alzheimers Dement 2017;13(4):406–18. doi: 10.1016/j.jalz.2016.07.152.
Benn, M., Nordestgaard, B.G., Tybjærg-Hansen, A. et al. Impact of glucose on risk of dementia: Mendelian randomisation studies in 115,875 individuals. Diabetologia 63, 1151–1161 (2020). https://doi.org/10.1007/s00125-020-05124-5
Bermejo‐Pareja, F., del Ser, T., Valentí, M., de la Fuente, M., Bartolome, F. and Carro, E., 2020. Salivary lactoferrin as biomarker for Alzheimer’s disease: Brain‐immunity interactions. Alzheimer’s & Dementia, [online] 16(8), pp.1196–1204. https://doi.org/10.1002/alz.12107.
Carro, E., Bartolomé, F., Bermejo-Pareja, F., Villarejo-Galende, A., Molina, J. A., Ortiz, P., Calero, M., Rabano, A., Cantero, J. L., & Orive, G. (2017). Early diagnosis of mild cognitive impairment and Alzheimer's disease based on salivary lactoferrin. Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring, 8, 131-138. https://doi.org/10.1016/j.dadm.2017.04.002
Cerasuolo, M., Di Meo, I., Auriemma, M.C., Trojsi, F., Maiorino, M.I., Cirillo, M., Esposito, F., Polito, R., Colangelo, A.M., Paolisso, G., Papa, M., & Rizzo, M.R. (2023). Iron and Ferroptosis More than a Suspect: Beyond the Most Common Mechanisms of Neurodegeneration for New Therapeutic Approaches to Cognitive Decline and Dementia. International Journal of Molecular Sciences, 24(11), 9637. https://doi.org/10.3390/ijms24119637
Crane, P.K., Walker, R., Hubbard, R.A., Li, G., Nathan, D.M., Zheng, H., Haneuse, S., Craft, S., Montine, T.J., Kahn, S.E., McCormick, W., McCurry, S.M., Bowen, J.D. and Larson, E.B., 2013. Glucose Levels and Risk of Dementia. New England Journal of Medicine, [online] 369(6), pp.540–548. https://doi.org/10.1056/nejmoa1215740.
Cunnane, S.C., Courchesne‐Loyer, A., St‐Pierre, V., Vandenberghe, C., Pierotti, T., Fortier, M., Croteau, E. and Castellano, C., 2016. Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer’s disease. Annals of the New York Academy of Sciences, [online] 1367(1), pp.12–20. https://doi.org/10.1111/nyas.12999.
Davis, J.J., Fournakis, N., & Ellison, J. (2020). Ketogenic Diet for the Treatment and Prevention of Dementia: A Review. Journal of Geriatric Psychiatry and Neurology. https://doi.org/10.1177/0891988720901785
Daulatzai, M.A., 2016. Cerebral hypoperfusion and glucose hypometabolism: Key pathophysiological modulators promote neurodegeneration, cognitive impairment, and Alzheimer’s disease. Journal of Neuroscience Research, [online] 95(4), pp.943–972. https://doi.org/10.1002/jnr.23777.
Dineley, K. T., Jahrling, J. B., & Denner, L. (2014). Insulin Resistance in Alzheimer's Disease. Neurobiology of Disease, 72PA, 92. https://doi.org/10.1016/j.nbd.2014.09.001
DiNicolantonio, J.J., Mangan, D. and O’Keefe, J.H., 2018. The fructose–copper connection: Added sugars induce fatty liver and insulin resistance via copper deficiency. Journal of Metabolic Health, [online] 3(1).
https://doi.org/10.4102/jir.v3i1.43.
Dugger, B.N., & Dickson, D.W. (2017). Pathology of Neurodegenerative Diseases. In Cold Spring Harbor Perspectives in Biology. Cold Spring Harbor Laboratory Press.
Fiest KM, Jetté N, Roberts JI, et al. The prevalence and incidence of dementia: A systematic review and meta-analysis. Can J Neurol Sci 2016;43 Suppl 1:S3–50. doi: 10.1017/cjn.2016.18.
Gammella, E., Recalcati, S., & Cairo, G. (2016). Dual role of ROS as signal and stress agents: iron tips the balance in favor of toxic effects. Oxidative Medicine and Cellular Longevity, 2016(1), 8629024.
Garrett, L. R., & Niccoli, T. (2022). Frontotemporal Dementia and Glucose Metabolism. Frontiers in Neuroscience, 16, 812222. https://doi.org/10.3389/fnins.2022.812222
González-Reyes RE, Aliev G, Ávila-Rodrigues M, Barreto GE. Alterations in Glucose Metabolism on Cognition: A Possible Link Between Diabetes and Dementia. Curr Pharm Des. 2016;22(7):812-8. doi: 10.2174/1381612822666151209152013. PMID: 26648470.
Gorelick, P.B., Scuteri, A., Black, S.E., DeCarli, C., Greenberg, S.M., Iadecola, C., Launer, L.J., Laurent, S., Lopez, O.L., Nyenhuis, D., Petersen, R.C., Schneider, J.A., Tzourio, C., Arnett, D.K., Bennett, D.A., Chui, H.C., Higashida, R.T., Lindquist, R., Nilsson, P.M., Roman, G.C., Sellke, F.W. and Seshadri, S., 2011. Vascular Contributions to Cognitive Impairment and Dementia. Stroke, [online] 42(9), pp.2672–2713. https://doi.org/10.1161/str.0b013e3182299496.
Grammatikopoulou, M.G., Goulis, D.G., Gkiouras, K., Theodoridis, X., Gkouskou, K.K., Evangeliou, A., Dardiotis, E., & Bogdanos, D.P. (2020). To Keto or Not to Keto? A Systematic Review of Randomized Controlled Trials Assessing the Effects of Ketogenic Therapy on Alzheimer Disease. Advances in Nutrition, 11(6), 1583–1602. https://doi.org/10.1093/advances/nmaa073
Hertz, L., Chen, Y. and Waagepetersen, H.S., 2015. Effects of ketone bodies in Alzheimer’s disease in relation to neural hypometabolism, β‐amyloid toxicity, and astrocyte function. Journal of Neurochemistry, [online] 134(1), pp.7–20. https://doi.org/10.1111/jnc.13107.
Huo, T., Jia, Y., Yin, C., Luo, X., Zhao, J., Wang, Z., & Lv, P. (2019). Iron dysregulation in vascular dementia: Focused on the AMPK/autophagy pathway. Brain Research Bulletin, 153, 305–313. https://doi.org/10.1016/j.brainresbull.2019.09.006
Kalaria, R. N. (2018). The pathology and pathophysiology of vascular dementia. Neuropharmacology, 134, 226-239. https://doi.org/10.1016/j.neuropharm.2017.12.030
Krikorian, R., Shidler, M. D., Dangelo, K., Couch, S. C., Benoit, S. C., & Clegg, D. J. (2012). Dietary ketosis enhances memory in mild cognitive impairment. Neurobiology of Aging, 33(2), 425.e19.
https://doi.org/10.1016/j.neurobiolaging.2010.10.006
Listabarth, S., König, D., Vyssoki, B. and Hametner, S., 2020. Does thiamine protect the brain from iron overload and alcohol‐related dementia? Alzheimer’s & Dementia, [online] 16(11), pp.1591–1595.
https://doi.org/10.1002/alz.12146.
Magaki, S., Raghavan, R., Mueller, C., Oberg, K.C., Vinters, H.V., & Kirsch, W.M. (2007). Iron, copper, and iron regulatory protein 2 in Alzheimer’s disease and related dementias. Neuroscience Letters, 418(1), 72–76. https://doi.org/10.1016/j.neulet.2007.02.077
Mohamed, W. A., Salama, R. M., & Schaalan, M. F. (2019). A pilot study on the effect of lactoferrin on Alzheimer’s disease pathological sequelae: Impact of the p-Akt/PTEN pathway. Biomedicine & Pharmacotherapy, 111, 714-723. https://doi.org/10.1016/j.biopha.2018.12.118
Moon, Y., Han, S.-H., & Moon, W.-J. (2016). Patterns of Brain Iron Accumulation in Vascular Dementia and Alzheimer’s Dementia Using Quantitative Susceptibility Mapping Imaging. Journal of Alzheimer’s Disease, 51(3), 737–745. https://doi.org/10.3233/jad-151037
Ohara, T., Doi, Y., Ninomiya, T., Hirakawa, Y., Hata, J., Iwaki, T., Kanba, S. and Kiyohara, Y., 2011. Glucose tolerance status and risk of dementia in the community. Neurology, [online] 77(12), pp.1126–1134. https://doi.org/10.1212/wnl.0b013e31822f0435.
Peloso GM, Beiser AS, Satizabal CL, et al. Cardiovascular health, genetic risk, and risk of dementia in the Framingham Heart Study. Neurology 2020;95(10):e1341–50. doi: 10.1212/WNL.0000000000010306.
Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimers Dement 2013;9(1):63–75.e2. doi: 10.1016/j.jalz.2012.11.007.
Raha, A.A., Biswas, A., Henderson, J., Chakraborty, S., Holland, A., Friedland, R.P., Mukaetova-Ladinska, E., Zaman, S. and Raha-Chowdhury, R., 2022. Interplay of Ferritin Accumulation and Ferroportin Loss in Ageing Brain: Implication for Protein Aggregation in Down Syndrome Dementia, Alzheimer’s, and Parkinson’s Diseases. International Journal of Molecular Sciences, [online] 23(3), p.1060.
https://doi.org/10.3390/ijms23031060.
Rawlings, A.M., Sharrett, A.R., Mosley, T.H., Ballew, S.H., Deal, J.A. and Selvin, E., 2017. Glucose Peaks and the Risk of Dementia and 20-Year Cognitive Decline. Diabetes Care, [online] 40(7), pp.879–886. https://doi.org/10.2337/dc16-2203.
Roubroeks, J.A.Y., Smith, R.G., van den Hove, D.L.A., & Lunnon, K. (2017). Epigenetics and DNA Methylomic Profiling in Alzheimer’s Disease and Other Neurodegenerative Diseases. Journal of Neurochemistry, 143, 158–170.
Shi L, Chen SJ, Ma MY, et al. Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep Med Rev 2018;40:4–16. doi: 10.1016/j.smrv.2017.06.010.
Siah, C. W., Ombiga, J., Adams, L. A., Trinder, D., & Olynyk, J. K. (2006). Normal Iron Metabolism and the Pathophysiology of Iron Overload Disorders. Clinical Biochemist Reviews, 27(1), 5-16.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1390789/
Wands, J. R. (2008). Alzheimer's Disease Is Type 3 Diabetes–Evidence Reviewed. Journal of Diabetes Science and Technology (Online), 2(6), 1101-1113. https://doi.org/10.1177/193229680800200619
Wu, C., Shapiro, L., Ouk, M., MacIntosh, B. J., Black, S. E., Shah, B. R., & Swardfager, W. (2022). Glucose-lowering drugs, cognition, and dementia: The clinical evidence. Neuroscience & Biobehavioral Reviews, 137, 104654. https://doi.org/10.1016/j.neubiorev.2022.104654
Zhao, Z. (2019). Iron and oxidizing species in oxidative stress and Alzheimer’s disease. Aging Medicine, 2(2), 82–87. https://doi.org/10.1002/agm2.12074
Anxiety: Causes, Symptoms, and Management
Key Takeaways: Anxiety can disrupt daily life when it becomes overwhelming. Common symptoms include restlessness, rapid heartbeat, and difficulty concentrating. Causes include stress, genetics, and…
Supporting Mental Health with Gut Health
Key Takeaways Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis. Probiotics: Beneficial bacteria that help regulate mood and support…
GABA (gamma-aminobutyric acid)
Key Takeaways GABA is a neurotransmitter that helps calm the nervous system. Low GABA levels can lead to anxiety, stress, and sleep problems. Natural precursors…
Reduce Stress through Pet Therapy
Key Highlights Pet therapy, or animal-assisted therapy, boosts health. Interacting with animals lowers cortisol, blood pressure, and heart rate. Therapy, service, and companion animals are…
Fight, Flight, Freeze, Fawn: Stress Response Examined
Key Takeaways The stress response includes four primary reactions, each serving as a survival mechanism. The fight response involves confronting the threat, often with aggression…
Alzheimer’s Disease: Symptoms, Causes, Treatment
Key Takeaways Alzheimer’s disease is a progressive neurodegenerative disorder affecting memory, thinking, and behavior. Oxidative stress, including from excess iron, plays a significant role in…
Emotional Freedom Technique (EFT): Tap to relieve stress
Key Highlights Learn about the origins and principles of Emotional Freedom Technique (EFT) for stress relief. Understand the science-backed mechanisms of how EFT works on…
Say Goodbye to Depression with Natural Remedies
Key Takeaways Regular exercise, sufficient sleep, and a diet full of bioavailable nutrients support mental health. Spending time in nature, like forest bathing and gardening,…
Mastering Emotional Healing: Your Guide to Recovery
Key Highlights Emotional healing is a gradual process requiring patience and self-compassion. Acknowledge and accept your feelings, and identify sources of emotional pain. Embrace vulnerability,…
Parkinson’s Disease : Symptoms, Causes & Treatment
Key Takeaways Parkinson’s disease is a progressive neurological disorder that affects movement and coordination. Oxidative stress and excess iron are significant factors in the progression…
Mental Benefits of Learning a New Language
Key Takeaways: Enhances brain volume and memory. Improves cognitive flexibility, multitasking, and executive functions. Delays cognitive decline and boosts emotional intelligence. Increases empathy, cultural awareness,…