Key Takeaways
- Increased Thirst and Urination: High blood sugar leads to dehydration, causing excessive thirst and frequent urination.
- Unexplained Weight Loss: Diabetes can cause the body to break down fat and muscle for energy, leading to sudden weight loss.
- Extreme Fatigue: The body’s inability to use glucose effectively results in persistent tiredness and low energy levels.
- Blurred Vision: Elevated blood sugar levels can affect the eyes, leading to blurred vision and potential long-term eye damage.
- Slow Healing and Infections: High glucose levels impair the body’s healing process, increasing the risk of infections and slow wound healing.
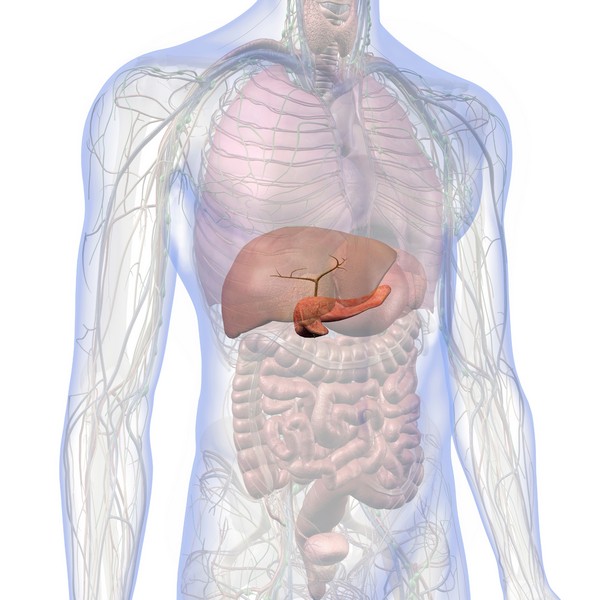
Diabetes is a chronic condition characterized by high levels of glucose in the blood. With millions of people affected globally, it poses a significant public health challenge.
Early detection is key to managing diabetes effectively and preventing serious complications.
Common Symptoms of Diabetes
Increased Thirst and Frequent Urination

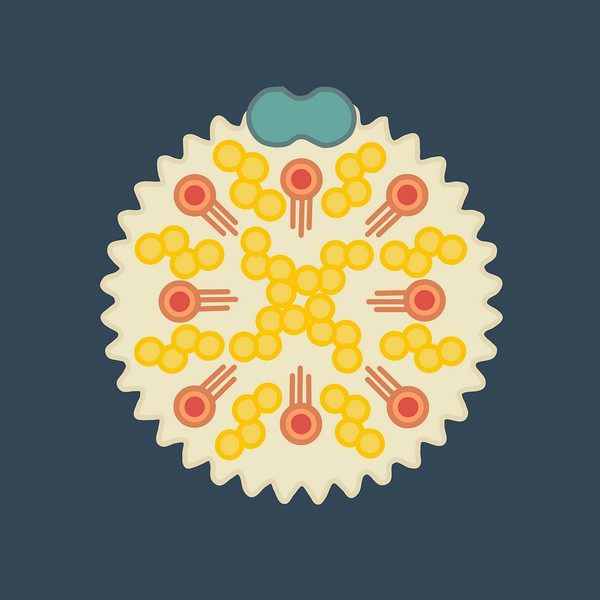
High blood sugar levels cause the kidneys to work overtime to filter and absorb excess glucose. When they can’t keep up, glucose is excreted into the urine, dragging along fluids from the tissues.
This leads to dehydration, which triggers increased thirst, and the cycle of frequent urination continues.
Extreme Fatigue
Diabetes interferes with the body’s ability to convert glucose into energy, leading to persistent tiredness.
Insulin resistance or insufficient insulin production means that glucose cannot enter the cells effectively, leaving you feeling fatigued even with adequate rest.
Unexplained Weight Loss
In diabetes, the body’s cells are starved of glucose, prompting the breakdown of fat and muscle tissue to meet energy needs.
This can lead to sudden and unexplained weight loss. This symptom is more commonly seen in type 1 diabetes, where insulin production is minimal or absent, but it can also occur in advanced cases of type 2 diabetes.
Blurred Vision

High blood sugar causes fluid to be pulled from the lenses of the eyes, affecting their ability to focus.
If left unchecked, prolonged high glucose levels can lead to more serious conditions such as diabetic retinopathy, which can threaten vision.
Slow Healing Wounds and Frequent Infections
Elevated glucose levels impair the function of the immune system, slowing down the body’s natural healing processes.
This makes individuals with diabetes more prone to infections, particularly in the skin and gums. Wounds may take longer to heal, and infections may become more frequent.
Increased Hunger
Despite high levels of glucose in the blood, cells in the body are not receiving it due to insulin resistance or deficiency.
This lack of energy triggers the brain to signal hunger, often leading to overeating. Paradoxically, this can result in weight gain even as other symptoms might cause weight loss.
Numbness or Tingling in Hands and Feet
Prolonged high blood sugar can damage nerves, leading to a condition known as diabetic neuropathy.
This often starts as numbness or a tingling sensation in the extremities, particularly the hands and feet.
If left untreated, it can progress to more severe nerve damage and loss of sensation.
Less Common Symptoms
Dark Patches of Skin
Acanthosis nigricans is characterized by dark, velvety patches of skin, often found in body folds such as the neck, armpits, and groin.
This condition is associated with insulin resistance and can be an early sign of type 2 diabetes.
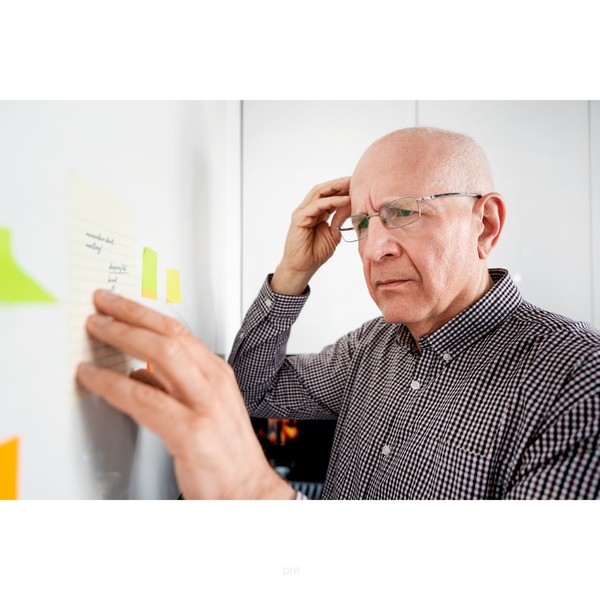
Irritability and Mood Changes

Fluctuations in blood sugar levels can have a significant impact on mood and mental health. People with diabetes may experience irritability, mood swings, or even symptoms of depression and anxiety.
Risk Factors and When to See a Doctor
Risk factors for diabetes include a family history of the condition, obesity, and a sedentary lifestyle. If you experience any of the symptoms mentioned, especially in combination, it’s important to seek medical evaluation.
Early diagnosis and management can prevent the progression of diabetes and reduce the risk of complications.
Conclusion
Recognizing the early signs of diabetes is essential for timely intervention and management.
If you notice any of these symptoms, consult a healthcare professional for a proper diagnosis and to discuss treatment options.
FAQ
What are the most common early signs of diabetes?
The most common early signs include increased thirst, frequent urination, unexplained weight loss, extreme fatigue, and blurred vision.
Can diabetes symptoms develop suddenly?
Yes, symptoms, especially in type 1 diabetes, can appear suddenly, while type 2 diabetes symptoms often develop more gradually.
How can I differentiate between type 1 and type 2 diabetes symptoms?
Type 1 diabetes often presents with sudden, severe symptoms like rapid weight loss and extreme fatigue. Type 2 symptoms are usually milder and develop over time, often associated with obesity and sedentary lifestyle.
What should I do if I experience these symptoms?
Seek medical advice immediately if you experience these symptoms. Early diagnosis is crucial for effective management and prevention of complications.
Research
Aigner, E., 2014. Dysregulation of iron and copper homeostasis in nonalcoholic fatty liver. World Journal of Hepatology, [online] 7(2), p.177. https://doi.org/10.4254/wjh.v7.i2.177.
Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-year Non-randomized Clinical Trial. Frontiers in Endocrinology. 2019; 10:348. doi: 10.3389/fendo.2019.00348.
Boden G, Sargrad K, Homko C, et al. Effect of a Low-Carbohydrate Diet on Appetite, Blood Glucose Levels, and Insulin Resistance in Obese Patients with Type 2 Diabetes. Ann Intern Med. 2005. https://doi.org/10.7326/0003-4819-142-6-200503150-00006.
Bruls, Y.M., de Ligt, M., Lindeboom, L., Phielix, E., Havekes, B., Schaart, G., Kornips, E., Wildberger, J.E., Hesselink, M.K., Muoio, D., Schrauwen, P. and Schrauwen-Hinderling, V.B., 2019. Carnitine supplementation improves metabolic flexibility and skeletal muscle acetylcarnitine formation in volunteers with impaired glucose tolerance: A randomised controlled trial. eBioMedicine, [online] 49, pp.318–330. https://doi.org/10.1016/j.ebiom.2019.10.017.
Courcoulas AP, Gallagher JW, Neiberg RH, et al. Bariatric Surgery vs Lifestyle Intervention for Diabetes Treatment: 5-Year Outcomes From a Randomized Trial. J Clin Endocrinol Metab. 2020 Mar 1;105(3):866–76. doi: 10.1210/clinem/dgaa006. PMID: 31917447; PMCID: PMC7032894.
de Souza, R.J., Mente, A., Maroleanu, A., Cozma, A.I., Ha, V., Kishibe, T., Uleryk, E., Budylowski, P., Schünemann, H., Beyene, J. and Anand, S.S., 2015. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ, [online] p.h3978. https://doi.org/10.1136/bmj.h3978.
Elliott RB, Harris DP, Hill JP, Bibby NJ, Wasmuth HE. Type I (insulin-dependent) diabetes mellitus and cow milk: casein variant consumption. Diabetologia. 1999 Mar;42(3):292-6. doi: 10.1007/s001250051153. Erratum in: Diabetologia 1999 Aug;42(8):1032. PMID: 10096780.
Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care 1 May 2019; 42 (5): 731–754. https://doi.org/10.2337/dci19-0014.
Feinman, R., 2016. Carbohydrates for people with diabetes is not cautious. Nutrition, [online] 32(1), pp.153–154. https://doi.org/10.1016/j.nut.2015.08.012.
Feinman RD, Pogozelski WK, Astrup A, Bernstein RK, Fine EJ, Westman EC, Accurso A, Frassetto L, Gower BA, McFarlane SI, Nielsen JV, Krarup T, Saslow L, Roth KS, Vernon MC, Volek JS, Wilshire GB, Dahlqvist A, Sundberg R, Childers A, Morrison K, Manninen AH, Dashti HM, Wood RJ, Wortman J, Worm N. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition. 2015 Jan;31(1):1-13. doi: 10.1016/j.nut.2014.06.011. Epub 2014 Jul 16. Erratum in: Nutrition. 2019 Jun;62:213. PMID: 25287761.
Fernández-Real, J.M., McClain, D. and Manco, M., 2015. Mechanisms Linking Glucose Homeostasis and Iron Metabolism Toward the Onset and Progression of Type 2 Diabetes. Diabetes Care, [online] 38(11), pp.2169–2176. https://doi.org/10.2337/dc14-3082.
Galloway, S.D.R., Craig, T.P. and Cleland, S.J., 2010. Effects of oral l-carnitine supplementation on insulin sensitivity indices in response to glucose feeding in lean and overweight/obese males. Amino Acids, [online] 41(2), pp.507–515. https://doi.org/10.1007/s00726-010-0770-5.
Gregg EW, Chen H, Wagenknecht LE, et al. Association of an Intensive Lifestyle Intervention With Remission of Type 2 Diabetes. JAMA. 2012;308(23):2489–2496. doi:10.1001/jama.2012.67929.
Haap, M., Machann, J., von Friedeburg, C., Schick, F., Stefan, N., Schwenzer, N.F., Fritsche, A., Häring, H.U. and Thamer, C., 2011. Insulin Sensitivity and Liver Fat: Role of Iron Load. The Journal of Clinical Endocrinology & Metabolism, [online] 96(6), pp.E958–E961. https://doi.org/10.1210/jc.2010-2682.
Huang, J., 2015. Association of insulin resistance with serum ferritin and aminotransferases-iron hypothesis. World Journal of Experimental Medicine, [online] 5(4), p.232.
https://doi.org/10.5493/wjem.v5.i4.232.
Krisai, P., Leib, S., Aeschbacher, S., Kofler, T., Assadian, M., Maseli, A., Todd, J., Estis, J., Risch, M., Risch, L. and Conen, D., 2016. Relationships of iron metabolism with insulin resistance and glucose levels in young and healthy adults. European Journal of Internal Medicine, [online] 32, pp.31–37. https://doi.org/10.1016/j.ejim.2016.03.017.
Lean ME, Leslie WS, Barnes AC, Brosnahan N, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet 2019 May 01.https://doi.org/10.1016/S2213-8587(19)30068-3.
Laugesen M, Elliott R. Ischaemic heart disease, Type 1 diabetes, and cow milk A1 beta-casein. N Z Med J. 2003 Jan 24;116(1168):U295. PMID: 12601419.
McLachlan CN. beta-casein A1, ischaemic heart disease mortality, and other illnesses. Med Hypotheses. 2001 Feb;56(2):262-72. doi: 10.1054/mehy.2000.1265. PMID: 11425301.
McKenzie AL, Hallberg SJ, Creighton BC, et al. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes. 2017 Mar 7;2(1):e5. doi: 10.2196/diabetes.6981. PMID: 30291062; PMCID: PMC6238887.
Molfino, A., Cascino, A., Conte, C., Ramaccini, C., Fanelli, F.R. and Laviano, A., 2010. Caloric Restriction and L‐Carnitine Administration Improves Insulin Sensitivity in Patients With Impaired Glucose Metabolism. Journal of Parenteral and Enteral Nutrition, [online] 34(3), pp.295–299. https://doi.org/10.1177/0148607109353440.
National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. Accessed at: https://www.cdc.gov/diabetes/data/statistics-report/index.html.
Okuyama, H., Langsjoen, P.H., Ohara, N., Hashimoto, Y., Hamazaki, T., Yoshida, S., Kobayashi, T. and Langsjoen, A.M., 2016. Medicines and Vegetable Oils as Hidden Causes of Cardiovascular Disease and Diabetes. Pharmacology, [online] 98(3–4), pp.134–170. https://doi.org/10.1159/000446704.
Rajpathak, S.N., Crandall, J.P., Wylie-Rosett, J., Kabat, G.C., Rohan, T.E. and Hu, F.B., 2009. The role of iron in type 2 diabetes in humans. Biochimica et Biophysica Acta (BBA) - General Subjects, [online] 1790(7), pp.671–681. https://doi.org/10.1016/j.bbagen.2008.04.005.
Riddle MC, Cefalu WT, Evans PH et al. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care 1 October 2021; 44 (10): 2438–2444. https://doi.org/10.2337/dci21-0034.
Robert M, Ferrand-Gaillard C, Disse E, et al. Predictive factors of type 2 diabetes remission 1 year after bariatric surgery: impact of surgical techniques. Obes Surg. 2013 Jun;23(6):770-5. doi: 10.1007/s11695-013-0868-4. PMID: 23355293.
Ruggenenti, P., Cattaneo, D., Loriga, G., Ledda, F., Motterlini, N., Gherardi, G., Orisio, S. and Remuzzi, G., 2009. Ameliorating Hypertension and Insulin Resistance in Subjects at Increased Cardiovascular Risk. Hypertension, [online] 54(3), pp.567–574. https://doi.org/10.1161/hypertensionaha.109.132522.
Stene, L.C., Joner, G. and Norwegian Childhood Diabetes Study Group, 2003. Use of cod liver oil during the first year of life is associated with lower risk of childhood-onset type 1 diabetes: a large, population-based, case-control study. The American journal of clinical nutrition, 78(6), pp.1128-1134.
Syrovatka, P., Kraml, P., Potockova, J., Fialova, L., Vejrazka, M., Crkovska, J. and Andel, M., 2009. Relationship between Increased Body Iron Stores, Oxidative Stress and Insulin Resistance in Healthy Men. Annals of Nutrition and Metabolism, [online] 54(4), pp.268–274. https://doi.org/10.1159/000229507.
Volk BM, McKenzie AL, Athinarayanan SJ, et al. A Population Shift in Meeting Glycemic Targets Following Five Years of a Very-Low-Carbohydrate Intervention (VLCI) and Continuous Remote Care (CRC) . Diabetes 1 June 2022; 71 (Supplement_1): 1176–P. https://doi.org/10.2337/db22-1176-P.
Wlazlo, N., van Greevenbroek, M.M.J., Ferreira, I., Jansen, E.H.J.M., Feskens, E.J.M., van der Kallen, C.J.H., Schalkwijk, C.G., Bravenboer, B. and Stehouwer, C.D.A., 2014. Iron metabolism is prospectively associated with insulin resistance and glucose intolerance over a 7-year follow-up period: the CODAM study. Acta Diabetologica, [online] 52(2), pp.337–348.
https://doi.org/10.1007/s00592-014-0646-3.
Zhou, X., Liu, R., Duan, S., Huang, G., Ye, Y. and Kong, Y., 2016. High Glucose Enhances oxLDL-Induced Apoptosis in Human Renal Proximal Tubular Epithelial Cells Largely via Inducing Lectin-Like ox-LDL Receptor-1. Pharmacology, [online] 98(1–2), pp.20–28. https://doi.org/10.1159/000444934.
Zhou, Z., Chen, G., Li, P., Rao, J., Wang, L., Yu, D., Lin, D., Fan, D., Ye, S., Wu, S., Gou, X., Wang, H., Guo, X., Lin, L., Suo, D. and Liu, Z., 2021. Prospective association of metal levels with gestational diabetes mellitus and glucose: A retrospective cohort study from South China. Ecotoxicology and Environmental Safety, [online] 210, p.111854.
https://doi.org/10.1016/j.ecoenv.2020.111854.
High Homocysteine: How to Manage Levels
Key Takeaways: Elevated homocysteine can raise the risk of heart disease and other health problems. Animal-based foods high in B vitamins help reduce homocysteine levels….
Is Eating Sugar Really That Bad For Your Health?
Should You Really Be Concerned? In short, YES! Thank you, that’s all folks, and do have a good evening. Seriously though, extensive research has established…
Atherosclerosis Prevention Strategies: Insights from Scientific Research
Key Takeaways Atherosclerosis is the hardening and narrowing of arteries caused by plaque buildup. Chronic inflammation and oxidative stress contribute to the development of plaque….
Alzheimer’s Disease: Symptoms, Causes, Treatment
Key Takeaways Alzheimer’s disease is a progressive neurodegenerative disorder affecting memory, thinking, and behavior. Oxidative stress, including from excess iron, plays a significant role in…
Insulin Resistance: What It Is & How to Manage It
Key Takeaways Insulin resistance leads to high blood sugar when cells stop responding to insulin. Often connected to obesity, poor diet, and physical inactivity. Symptoms…
Iron Overload: Symptoms & Prevention Tips
Key Takeaways: Iron overload happens when the body absorbs excessive iron, which can damage organs. Common symptoms include fatigue, joint pain, and skin changes. Early…
Metabolic Syndrome: Managing This Health Risk
Key Takeaways Metabolic syndrome is a cluster of conditions increasing the risk of heart disease, stroke, and diabetes. Symptoms include high blood pressure, high blood…
Inflammation: Causes & Effects
Key Takeaways Inflammation is the body’s response to injury or infection, but chronic inflammation can lead to health problems. Iron overload from artificial sources and…
L-Glutamine and Gut Health: Benefits and Side Effects
Key Takeaways L-Glutamine is essential for gut health. Benefits include improved digestion and reduced inflammation. Potential side effects are rare but can occur in high…
Coping with Pet Allergies: Tips & Advice
Key Highlights Pet allergies often cause sneezing, coughing, itchy eyes, and skin rash. Pet allergens are in the saliva, urine, and dander of furry animals….
Supporting Mental Health with Gut Health
Key Takeaways Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis. Probiotics: Beneficial bacteria that help regulate mood and support…
Diabetes: Everything You Need to Know
Key Takeaways Type 1 and Type 2 diabetes involve insulin regulation issues, with Type 2 being the most common due to insulin resistance. Copper, retinol,…
Histamine: What You Should Know
Key Takeaways Histamine’s Role: Vital in immune responses, digestion, and as a neurotransmitter in the central nervous system. Histamine Production: Produced in mast cells and…
Travel Hygiene Tips: Stay Fresh on the Go
Key Highlights Key practices include frequent handwashing, showering, and oral care. Packing a portable hygiene kit can help you stay fresh on the go. Advanced…
Metabolic Health: What It Means and How to Improve It
Key Takeaways Metabolic health reflects how well your body processes energy and maintains stable blood sugar, cholesterol, and blood pressure. Key indicators of metabolic health…
7 Remedies for Kidney Stones: A Comprehensive Guide
Key Takeaways Staying well-hydrated and adopting a balanced diet can help prevent kidney stones. Knowing the causes of kidney stones can inform effective prevention strategies….
Uric Acid: Effects & Management
7 Simple Tips for Lowering Blood Pressure Naturally
Maintaining healthy blood pressure levels is essential for overall well-being, as high blood pressure can lead to serious health complications. However, it is possible to…
Vegetable Oil: Health Risks You Might Not Know
Key Takeaways: Omega-6 fats from vegetable oils cause oxidative stress and inflammation. Reducing omega-6 intake and using stable fats can lower health risks. High triglycerides…
Postbiotics: What They Are and Why They Are Important
Key Takeaways Postbiotics 101: They’re beneficial by-products from probiotics that consume prebiotics Boosts Immunity: Postbiotics sharpen your immune system, helping fight off pathogens and reducing…
Dialysis: Benefits & Challenges
Key Takeaways Dialysis removes waste and excess fluid from the blood when kidneys cannot function. Two main types: hemodialysis (machine-based) and peritoneal dialysis (abdomen-based). Dialysis…
Non-Alcoholic Fatty Liver Disease (NAFLD)
Key Takeaways NAFLD involves fat buildup in the liver not caused by alcohol. Commonly associated with obesity, insulin resistance, and metabolic syndrome. NAFLD can lead…
Parkinson’s Disease : Symptoms, Causes & Treatment
Key Takeaways Parkinson’s disease is a progressive neurological disorder that affects movement and coordination. Oxidative stress and excess iron are significant factors in the progression…
Chronic Kidney Disease (CKD): Causes & Treatment
Key Takeaways Ultra-processed foods and high carbohydrate intake worsen inflammation, harming kidney function. Iron overload leads to oxidative stress, which accelerates CKD progression. Copper is…
Boost Insulin Sensitivity Naturally
Key Takeaways Improving insulin sensitivity helps control blood sugar and reduces the risk of metabolic disorders. Regular physical activity enhances how cells respond to insulin….
Allergy-Friendly Pets
Key Highlights Hypoallergenic pets are great for people with pet allergies, as they produce fewer allergens like dander, saliva, and proteins that can trigger symptoms….
Triglycerides: Levels & Range Explained
Key Highlights Triglycerides are the most common form of fat in the body play a role in energy storage High levels of triglycerides can increase…
Remnant Cholesterol (RC): Its Origins & Impact
Key Takeaways Remnant cholesterol (RC) is the cholesterol content left in the blood after triglycerides are removed from VLDL and IDL particles. RC is a…
Quit Sugar for 14 Days: What Happens to Your Body?
Key Takeaways: Immediate Health Benefits of Reducing Sugar: In just two weeks, enjoy enhanced energy levels, weight loss, a reduced risk of chronic diseases, and…
Alcohol and Its Effects
Key Takeaways Alcohol is metabolized primarily in the liver, producing acetaldehyde, a toxic byproduct. Chronic alcohol consumption leads to liver damage, including fatty liver, hepatitis,…
Proteolytic Enzymes and Heart Health: What the Research Shows
Your heart works tirelessly to pump blood throughout your body, delivering essential nutrients and oxygen to your cells. However, factors like poor diet, stress, and…
How to Lower Triglycerides Fast: Natural Solutions
Key Highlights Triglycerides, a type of fat found in the blood, are essential indicators of metabolic health. Elevated triglyceride levels increase the risk of heart…
SIBO Bloating: Causes, Diet, & Management Tips
Key Takeaways SIBO disrupts gut bacteria balance, causing bloating, pain, and nutrient absorption issues. Symptoms include bloating, abdominal pain, diarrhea, constipation, weight loss, and fatigue….