Key Takeaways
- Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis.
- Probiotics: Beneficial bacteria that help regulate mood and support cognitive function.
- Diet’s Role: Food choices have a significant impact on gut balance and mental health.
- Prebiotics: Nourishing gut bacteria with prebiotics can boost mental wellness.
- Lifestyle Influence: Stress management, sleep, and exercise are essential for maintaining a healthy gut and mind.
Introduction
Gut health significantly influences mental wellbeing. The gut-brain axis connects the digestive system with the brain, showing how a healthy gut supports mental clarity and emotional stability.
This connection is shaped by factors such as diet, probiotics, prebiotics, and lifestyle choices.
The Gut-Brain Connection
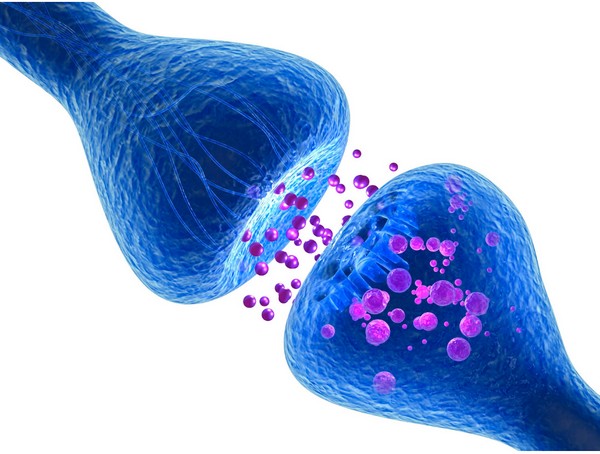
The gut-brain axis is a communication network linking the gut and the brain. This connection involves neurotransmitters, gut hormones, and the vagus nerve.
Imbalances in gut bacteria, known as dysbiosis, can lead to mood disorders like anxiety and depression. Maintaining a balanced gut environment is essential for mental wellness.
Probiotics and Mental Wellbeing
Probiotics are live bacteria that support a healthy gut environment. Certain probiotic strains, such as Lactobacillus and Bifidobacterium, influence the production of neurotransmitters like serotonin and GABA.
These neurotransmitters play a key role in regulating mood and reducing stress.
Diet’s Impact on Gut and Mental Health

Diet directly affects both gut health and mental wellbeing. A nutrient-rich diet supports a healthy gut, which in turn influences mood and cognitive function.
Ultra-processed foods, high sugar intake, and excessive carbohydrates can disrupt gut balance, leading to inflammation and negative effects on mental health.
Eating probiotic-rich foods, such as yogurt, kefir, and fermented vegetables, or taking supplements can help maintain a balanced gut microbiome, supporting mental health.
Foods like fermented vegetables, healthy fats, and complete proteins are particularly beneficial for gut health.
Prebiotics and Mental Wellbeing
Prebiotics are non-digestible fibers that nourish probiotics. These fibers help maintain a balanced gut environment, which is important for mental health.
Foods rich in prebiotics, such as garlic, onions, and leeks, can be included in the diet to support gut health.
Prebiotic supplements may also enhance the gut-brain connection and contribute to overall mental wellness.
Lifestyle Factors

Lifestyle choices are important in supporting both gut and mental health.
- Managing stress through techniques like meditation and deep breathing helps maintain gut balance.
- Regular exercise promotes a healthy gut microbiome and enhances mood.
- Adequate sleep is also essential for gut health, as it allows the body to repair and maintain a balanced gut environment, which positively impacts mental resilience.
Conclusion
Maintaining optimal gut health is helpful for promoting mental well-being. There is not necessarily one approach that would be ideal for every person. With multiple options available to adjust lifestyle choices, the answer is within reach. Understanding the gut-brain connection and making informed dietary and lifestyle choices supports mental health and overall quality of life.
FAQ
How does gut health affect mental wellbeing?
Gut health influences mental wellness through the gut-brain axis, impacting mood, stress levels, and cognitive function.
What are the best foods for supporting gut and mental health?
Fermented foods, healthy fats, and complete proteins are excellent for supporting both gut and mental health.
Can probiotics help with anxiety and depression?
Yes, certain probiotic strains support mood regulation and reduce symptoms of anxiety and depression.
How does stress impact gut health and mental wellness?
Stress disrupts the gut microbiome, leading to digestive issues and negatively affecting mental health.
What lifestyle changes can improve both gut and mental health?
Adopting stress management techniques, regular exercise, and quality sleep into your routine supports both gut and mental health.
Research
(2012). Structure, function and diversity of the healthy human microbiome. Nature, 486(7402), 207-214.
https://www.nature.com/articles/nature11234
Appleton, J. (2018). The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integrative Medicine: A Clinician's Journal, 17(4), 28-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469458/
Bercik P, Denou E, Collins J, et al. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology. 2011;141(2):599-609.
Borrelli L, Aceto S, Agnisola C., et al. Probiotic modulation of the microbiota-gut-brain axis and behaviour in zebrafish. Sci Rep. 2016;6:30046.
Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203-209.
Collins SM, Kassam Z, Bercik P. The adoptive transfer of behavioral phenotype via the intestinal microbiota: Experimental evidence and clinical implications. Curr Opin Microbiol. 2013;16:240-245.
Cryan JF, Dinan TG. Mind-altering microorganisms: The impact of the gut microbiota on brain and behavior. Nat Rev Neurosci. 2012;13:701-712.
Douglas-Escobar M, Elliott E, Neu J. Effect of intestinal microbial ecology on the developing brain. JAMA Pediatr. 2013;167:374-379.
Forbes JD, Bernstein C.N., Tremlett, H., Van Domselaar, G. and Knox, N.C. A fungal world: could the gut mycobiome be involved in neurological disease? Frontiers in microbiology. 2019;9:3249.
Foster JA, McVey Neufeld KA. Gut-brain axis: How the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305-312.
Goehler LE, Gaykema RP, Opitz N, Reddaway R, Badr N, Lyte M. Activation in vagal afferents and central autonomic pathways: Early responses to intestinal infection with Campylobacter jejuni. Brain Behav Immun. 2005;19:334-344.
Kennedy PJ, Clarke G, Quigley EM, Groeger JA, Dinan TG, Cryan JF. Gut memories: Towards a cognitive neurobiology of irritable bowel syndrome. Neurosci Biobehav Rev. 2012;36:310-340.
Lyte M. Microbial endocrinology in the microbiome-gut-brain axis: How bacterial production and utilization of neurochemicals influence behavior. PLOS Pathog. 2013;9:e1003726.
Lyte M, Varcoe JJ, Bailey MT. Anxiogenic effect of subclinical bacterial infection in mice in the absence of overt immune activation. Physiol Behav. 1998;65:63-68.
Long-Smith, C., O’Riordan, K.J., Clarke, G., Stanton, C., Dinan, T.G. and Cryan, J.F. Microbiota-Gut-Brain Axis: New Therapeutic Opportunities. Annual Review of Pharmacology and Toxicology. 2020;60(1):477–502.
Mayer EA, Padua D, Tillisch K. Altered brain‐gut axis in autism: Comorbidity or causative mechanisms? BioEssays. 2014;36(10):933–939.
Mayer EA, Savidge T, Shulman RJ. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500-1512.
Mayer, E.A., Tillisch, K. and Gupta, A., 2015. Gut/brain axis and the microbiota. Journal of Clinical Investigation, [online] 125(3), pp.926–938.
https://doi.org/10.1172/jci76304.
Mayer, E.A., 2011. Gut feelings: the emerging biology of gut–brain communication. Nature Reviews Neuroscience, [online] 12(8), pp.453–466.
https://pubmed.ncbi.nlm.nih.gov/21750565/.
McVey Neufeld KA, Mao YK, Bienenstock J, Foster JA, Kunze WA. The microbiome is essential for normal gut intrinsic primary afferent neuron excitability in the mouse. Neurogastroenterol Motil. 2013;25(2):183-188.
Noble EE, Hsu TM, Kanoski SE. Gut to brain dysbiosis: Mechanisms linking Western diet consumption, the microbiome, and cognitive impairment. Front Behav Neurosci. 2017;11-19.
Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain–gut–enteric microbiota axis. Nature Reviews Gastroenterology & Hepatology. 2009;6(5). https://doi.org/10.1038/nrgastro.2009.35
Sender R, Fuchs S, Milo R. Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans. Cell. 2016;164(3):337-340.
Shkoporov AN, Hill C. Bacteriophages of the human gut: the “known unknown” of the microbiome. Cell host & microbe. 2019;25(2):195-209.
Sudo N, Chida Y, Aiba Y, et al. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol. 2004;558(Pt 1):263-275.
Wang HX, Wang YP. Gut microbiota-brain axis. Chinese Medical Journal. 2016;129(19):2373-2380.
Postbiotics: What They Are and Why They Are Important
Key Takeaways Postbiotics 101: They’re beneficial by-products from probiotics that consume prebiotics Boosts Immunity: Postbiotics sharpen your immune system, helping fight off pathogens and reducing…
SIBO Bloating: Causes, Diet, & Management Tips
Key Takeaways SIBO disrupts gut bacteria balance, causing bloating, pain, and nutrient absorption issues. Symptoms include bloating, abdominal pain, diarrhea, constipation, weight loss, and fatigue….
L-Glutamine and Gut Health: Benefits and Side Effects
Key Takeaways L-Glutamine is essential for gut health. Benefits include improved digestion and reduced inflammation. Potential side effects are rare but can occur in high…