Key Takeaways
- Dialysis removes waste and excess fluid from the blood when kidneys cannot function.
- Two main types: hemodialysis (machine-based) and peritoneal dialysis (abdomen-based).
- Dialysis does not cure kidney disease but helps manage symptoms.
- Nutrition and fluid management are critical for dialysis patients.
- Each dialysis type has different benefits, risks, and lifestyle implications.
What is Dialysis?
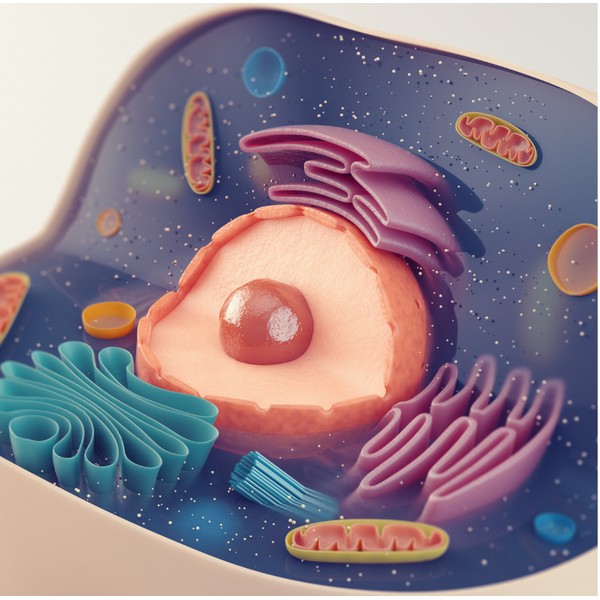
Definition and Purpose of Dialysis
Dialysis is a medical procedure that removes waste, toxins, and excess fluids from the blood when the kidneys are no longer functioning properly. It helps restore the body’s balance of fluids and electrolytes.
Why Dialysis is Necessary for Kidney Failure
When the kidneys lose their ability to filter blood effectively, harmful waste products accumulate, leading to serious health issues. Dialysis acts as an artificial replacement to perform these vital functions.
Types of Dialysis

Hemodialysis
Hemodialysis involves using a machine to filter the blood outside the body. The process typically occurs at a dialysis center or sometimes at home.
How Hemodialysis Works
During hemodialysis, blood is taken from the body, filtered through a dialyzer (artificial kidney), and then returned clean to the body. This process is usually done three times per week for 3-4 hours per session.
Pros and Cons of Hemodialysis
Pros:
- Effective in removing waste quickly.
- Usually supervised by healthcare professionals.
Cons: - Requires regular visits to a dialysis center.
- Can cause fatigue and blood pressure fluctuations.
Peritoneal Dialysis
Peritoneal dialysis uses the lining of the abdomen (peritoneum) to filter blood. A dialysis solution is introduced into the abdominal cavity and absorbs waste products from the blood.
How Peritoneal Dialysis Works
The dialysis solution is infused into the abdomen, where it stays for several hours, absorbing waste. The fluid is then drained and replaced. This can be done multiple times daily or overnight while sleeping.
Pros and Cons of Peritoneal Dialysis
Pros:
- Can be done at home, offering more flexibility.
- Less dietary and fluid restrictions.
Cons: - Risk of infections in the abdominal cavity.
- Requires strict hygiene and maintenance of the catheter.
Choosing the Right Type of Dialysis

Factors to Consider When Choosing Dialysis
The choice between hemodialysis and peritoneal dialysis depends on factors like lifestyle, medical condition, and personal preference. Patients should consult their healthcare providers to find the best fit for their needs.
Benefits and Risks of Each Method
Both methods are effective, but each comes with unique benefits and risks. Hemodialysis offers faster results but may be less convenient, while peritoneal dialysis provides flexibility but requires more self-care.
Living with Dialysis
Managing Day-to-Day Life with Dialysis
Dialysis requires significant lifestyle adjustments, including managing treatment schedules, avoiding certain foods, and maintaining regular healthcare checkups.
Nutritional Needs for Dialysis Patients
Patients need to follow a specific diet to maintain health, typically focusing on controlled fluid intake, moderate potassium and sodium, and ensuring enough protein to support bodily functions.
Challenges and Complications

Common Side Effects of Dialysis
Patients may experience fatigue, muscle cramps, low blood pressure, and infection risks depending on the type of dialysis.
Infection Risks and Preventative Measures
Proper care of the dialysis access point (fistula, catheter, or abdominal port) is essential to prevent infections like peritonitis in peritoneal dialysis or sepsis in hemodialysis.
Innovations in Dialysis Treatment
Recent Advances in Dialysis Technology
New technologies such as wearable dialysis machines and more efficient home dialysis options are improving the quality of life for patients with kidney failure.
Future of Kidney Replacement Therapies
Researchers are exploring alternatives like bioengineered kidneys and advances in regenerative medicine, offering hope for better solutions in kidney disease treatment.
FAQ
What is the main purpose of dialysis?
Dialysis replaces the kidney’s filtering function by removing waste and excess fluid from the blood.
How often do dialysis patients need treatment?
Hemodialysis is typically needed three times per week, while peritoneal dialysis can be performed daily.
What are the main differences between hemodialysis and peritoneal dialysis?
Hemodialysis is done via a machine, usually in a center, while peritoneal dialysis uses the abdominal lining at home to filter blood.
Can dialysis completely replace kidney function?
No, dialysis helps manage symptoms but does not fully replace the kidney’s ability to regulate waste and fluid.
Are there any risks involved with dialysis treatment?
Yes, potential risks include infections, low blood pressure, fatigue, and complications related to access points for dialysis.
Research
Agarwal, R., Vasavada, N., Sachs, N.G. & Chase, S. (2004). Oxidative stress and renal injury with intravenous iron in patients with chronic kidney disease. Kidney International, 65(6), pp.2279–2289. https://doi.org/10.1111/j.1523-1755.2004.00648.x
Avesani, C.M., Cuppari, L., Nerbass, F.B., Lindholm, B. & Stenvinkel, P. (2023). Ultraprocessed foods and chronic kidney disease—double trouble. Clinical Kidney Journal, 16(11), pp.1723–1736. https://doi.org/10.1093/ckj/sfad103
Banegas, J.R. (2023). Ultra-Processed Food Consumption is Associated with Renal Function Decline in Older Adults: A Prospective Cohort Study. Nutrients, 13(2), 428. https://doi.org/10.3390/nu13020428
Basturk, T. & Unsal, A. (2011). WHAT IS THE FREQUENCY OF CARBOHYDRATE METABOLISM DISORDER IN CKD? Journal of Renal Care, 38(1), pp.15–21. https://doi.org/10.1111/j.1755-6686.2011.00246.x
Cai, Q., Duan, M.-J., Dekker, L.H., Carrero, J.J., Avesani, C.M., Bakker, S.J., de Borst, M.H. & Navis, G.J. (2022). Ultraprocessed food consumption and kidney function decline in a population-based cohort in the Netherlands. The American Journal of Clinical Nutrition, 116(1), pp.263–273. https://doi.org/10.1093/ajcn/nqac073
Cai, Q., Duan, M., Dekker, L.H., Bakker, S.J., De Borst, M. & Navis, G. (2021). FC 081 ULTRA-PROCESSED FOOD CONSUMPTION AND RISK OF INCIDENT CHRONIC KIDNEY DISEASE: THE LIFELINES COHORT. Nephrology Dialysis Transplantation, 36(Supplement_1). https://doi.org/10.1093/ndt/gfab139.001
Du, S., Kim, H., Crews, D.C., White, K. & Rebholz, C.M. (2022). Association Between Ultraprocessed Food Consumption and Risk of Incident CKD: A Prospective Cohort Study. American Journal of Kidney Diseases, 80(5), pp.589-598.e1. https://doi.org/10.1053/j.ajkd.2022.03.016
Erdemli, Z., Gul, M., Kayhan, E., Gokturk, N., Bag, H.G. & Erdemli, M.E. (2024). High-Fat and Carbohydrate Diet Caused Chronic Kidney Damage by Disrupting Kidney Function, Caspase-3, Oxidative Stress and Inflammation. Prostaglandins & Other Lipid Mediators, 172, p.106822. https://doi.org/10.1016/j.prostaglandins.2024.106822
Fishbane, S., Kalantar‐Zadeh, K. & Nissenson, A.R. (2004). Serum Ferritin in Chronic Kidney Disease: Reconsidering the Upper Limit for Iron Treatment. Seminars in Dialysis, 17(5), pp.336–341. https://doi.org/10.1111/j.0894-0959.2004.17359.x
Friedman, A.N., Ogden, L.G., Foster, G.D., Klein, S., Stein, R., Miller, B., Hill, J.O., Brill, C., Bailer, B., Rosenbaum, D.R. & Wyatt, H.R. (2012). Comparative Effects of Low-Carbohydrate High-Protein Versus Low-Fat Diets on the Kidney. Clinical Journal of the American Society of Nephrology, 7(7), pp.1103–1111. https://doi.org/10.2215/cjn.11741111
Ganz, T. & Nemeth, E. (2016). Iron Balance and the Role of Hepcidin in Chronic Kidney Disease. Seminars in Nephrology, 36(2), pp.87–93. https://doi.org/10.1016/j.semnephrol.2016.02.001
Gaweda, A.E. (2017). Markers of iron status in chronic kidney disease. Hemodialysis International, 21(S1). https://doi.org/10.1111/hdi.12556
Gersch, M. S., Mu, W., Cirillo, P., Reungjui, S., Zhang, L., Roncal, C., Sautin, Y. Y., Johnson, R. J., & Nakagawa, T. (2007). Fructose, but not dextrose, accelerates the progression of chronic kidney disease. American Journal of Physiology-Renal Physiology.
https://doi.org/F-00181-2007
Gu, Y., Li, H., Ma, H., Zhang, S., Meng, G., Zhang, Q., Liu, L., Wu, H., Zhang, T., Wang, X., Zhang, J., Sun, S., Wang, X., Zhou, M., Jia, Q., Song, K., Liu, Q., Huang, T., Borné, Y., Wang, Y., Qi, L. & Niu, K. (2023). Consumption of Ultraprocessed Food and Development of Chronic Kidney Disease: The Tianjin Chronic Low-Grade Systemic Inflammation and Health and UK Biobank Cohort Studies. The American Journal of Clinical Nutrition, 117(2), pp.373–382. https://doi.org/10.1016/j.ajcnut.2022.11.005
He, X., Zhang, X., Si, C., Feng, Y., Zhu, Q., Li, S., & Shu, L. (2024). Ultra-processed food consumption and chronic kidney disease risk: A systematic review and dose–response meta-analysis. Frontiers in Nutrition, 11, 1359229.
https://doi.org/10.3389/fnut.2024.1359229
Jardim, M.Z., Costa, B.V. de L., Pessoa, M.C. & Duarte, C.K. (2021). Ultra-Processed Foods Increase Noncommunicable Chronic Disease Risk. Nutrition Research, 95, pp.19–34. https://doi.org/10.1016/j.nutres.2021.08.006
Juraschek, S.P., Appel, L.J., Anderson, C.A. & Miller, E.R. (2013). Effect of a High-Protein Diet on Kidney Function in Healthy Adults: Results From the OmniHeart Trial. American Journal of Kidney Diseases, 61(4), 547-554. https://doi.org/10.1053/j.ajkd.2012.10.017
Javier, V., Jesús, D., & Francisco, J. The Burden of Carbohydrates in Health and Disease. Nutrients, 14(18), 3809.
https://doi.org/10.3390/nu14183809
Kaburagi, T., Kanaki, K., Otsuka, Y. & Hino, R. (2019). Low-Carbohydrate Diet Inhibits Different Advanced Glycation End Products in Kidney Depending on Lipid Composition but Causes Adverse Morphological Changes in a Non-Obese Model Mice. Nutrients, 11(11), p.2801. https://doi.org/10.3390/nu11112801
Kalantar-Zadeh, K., Jafar, T.H., Nitsch, D., Neuen, B.L. & Perkovic, V. (2021). Chronic Kidney Disease. The Lancet, 398(10302), pp.786–802. https://doi.org/10.1016/s0140-6736(21)00519-5
Kleinknecht, C., Laouari, D., Hinglais, N., Habib, R., Dodu, C., Lacour, B., Broyer, M., Nalbandian, W.T.A.O.E. & Lacoste, M. (1986). Role of Amount and Nature of Carbohydrates in the Course of Experimental Renal Failure. Kidney International, 30(5), 687-693. https://doi.org/10.1038/ki.1986.241
Kim, H., Lee, H., Kwon, S.H., Jeon, J.S., Noh, H., Han, D.C. & Kim, H. (2021). Relationship Between Carbohydrate-to-Fat Intake Ratio and the Development of Chronic Kidney Disease: A Community-Based Prospective Cohort Study. Clinical Nutrition, 40(10), pp.5346–5354. https://doi.org/10.1016/j.clnu.2021.09.001
Kityo, A. & Lee, S.-A. (2022). The Intake of Ultra-Processed Foods and Prevalence of Chronic Kidney Disease: The Health Examinees Study. Nutrients, 14(17), p.3548. https://doi.org/10.3390/nu14173548
Lima, T.G., Benevides, F.L.N., Esmeraldo Filho, F.L., Farias, I.S., Dourado, D.X.C., Fontenele, E.G.P., Moraes, M.E.A. & Quidute, A.R.P. (2019). Treatment of Iron Overload Syndrome: A General Review. Rev Assoc Med Bras (1992), 65(9), 1216-1222. https://doi.org/10.1590/1806-9282.65.9.1216
Liu, M., Yang, S., Ye, Z., Zhang, Y., Zhang, Y., He, P., Zhou, C.,
Li, J. & Ding, J. (2023). Dietary Carbohydrate Intake and Risk of Incident Chronic Kidney Disease in a Chinese Population. Nutrients, 15(1), p.137. https://doi.org/10.3390/nu150100137
Nair, V., Li, X., Weiss, C., Zelnick, L., Hou, F., Clevenger, B., Obeid, A., He, J., Wood, C., Sharma, S., Ellis, B., Dey, N., Mehrotra, R., Cizman, B. & Garonzik-Wang, J.M. (2022). Association Between Carbohydrate Intake and the Risk of Chronic Kidney Disease: A Retrospective Cohort Study. American Journal of Kidney Diseases, 79(1), pp.58–65. https://doi.org/10.1053/j.ajkd.2021.05.013
Nguyen, D., Hoang, P. & Phan, H. (2017). High Carbohydrate Diet Promotes Chronic Kidney Disease Progression by Affecting the Metabolic Pathways. Kidney International Supplements, 7(1), pp.32–37. https://doi.org/10.1016/j.kisu.2017.01.001
Peyton, S.C. & Spiegelman, D. (2022). Dietary Carbohydrate Intake and Incidence of Chronic Kidney Disease: A Prospective Study. Journal of Renal Nutrition, 32(1), pp.33–43. https://doi.org/10.1053/j.jrn.2021.08.002
Ren, Q., Zhou, Y., Luo, H., Chen, G., Han, Y., Zheng, K., Qin, Y. & Li, X. (2023). Associations of Low-Carbohydrate with Mortality in Chronic Kidney Disease. Renal Failure, 45(1). https://doi.org/10.1080/0886022x.2023.2202284
Smith, A. & Walker, M. (2023). High-Fat Diet and Risk of Chronic Kidney Disease: A Longitudinal Study. Nutrition, 99, pp.1-8. https://doi.org/10.1016/j.nut.2022.111088
Wish, J.B., Aronoff, G.R., Bacon, B.R., Brugnara, C., Eckardt, K.-U., Ganz, T., Macdougall, I.C., Núñez, J., Perahia, A.J. and Wood, J.C., 2018. Positive Iron Balance in Chronic Kidney Disease: How Much is Too Much and How to Tell? American Journal of Nephrology, [online] 47(2), pp.72–83.
https://doi.org/10.1159/000486968.
Zainordin, N.A., Eddy Warman, N.A., Mohamad, A.F., Abu Yazid, F.A., Ismail, N.H., Chen, X.W., Koshy, M., Abdul Rahman, T.H., Mohd Ismail, N. & Abdul Ghani, R. (2021). Safety and Efficacy of Very Low Carbohydrate Diet in Patients with Diabetic Kidney Disease—A Randomized Controlled Trial. PLOS ONE, 16(10), p.e0258507. https://doi.org/10.1371/journal.pone.0258507
Adrenal Fatigue: Symptoms & Prevention
Key Takeaways: Adrenal fatigue is often linked to prolonged stress, leading to tiredness, brain fog, and mood swings. Disruptions in cortisol production can affect energy,…
DNA & Longevity: Can You Live to 200?
Key Takeaways: Longevity is shaped by a mix of genetics and lifestyle. Certain genes are linked to longer lifespans. Lifestyle choices can influence how long…
Adrenal Cocktail: Recipe and Benefits
Key Takeaways The adrenal cocktail supports adrenal health and maintains energy levels. Combines potassium, sodium, and vitamin C for effective adrenal nourishment. Consumed in the…
Sunburn Prevention: Holistic and Natural Approaches
Key Takeaways A poor diet increases the risk of sunburn and skin damage. Short, regular sun exposure reduces the risk of sunburn. Early morning and…
Why Sunlight is Essential for a Healthy Life
Key Takeaways Sunlight helps the body produce vitamin D, supporting bone health and immune function. Exposure to sunlight can improve mood and reduce symptoms of…
Managing Menopause Symptoms – A Guide to Navigate this Life Stage
Exercise RoutineManaging Stress Improving Sleep HabitsSeeking Emotional Support:Adjusting Your DietConsidering Alternative TherapiesFrequently Asked Questions Menopause is a natural stage in a woman’s life marking the…
Natural Remedies for Common Ailments: From Headaches to Allergies
Key Takeaways The appeal of natural remedies lies in their holistic approach, fewer side effects, and environmental sustainability. Specific natural remedies can effectively alleviate common…
Diatomaceous Earth: Natural Uses & Benefits
Key Takeaways – Diatomaceous earth is a natural powder made from fossilized algae called diatoms. – It helps cleanse the body of toxins and heavy…
Fluoride: Risks & Controversies
Key Takeaways Fluoride is widely used in dental products and water supplies, but its safety is debated. Overexposure to fluoride can lead to conditions like…
Bromate: Its Impact on Your Thyroid & Nervous System
Key Takeaways Bromate is a toxic byproduct from water disinfection, impacting thyroid and nervous system health. It interferes with iodine, leading to thyroid dysfunction and…
Autism: Causes, Symptoms, and Management
Key Takeaways Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition that varies widely in symptoms and severity. Both genetic and environmental factors contribute to…
The Randle Cycle: Glucose Fat Energy Dilemma
Key Takeaways The Randle Cycle explains how the body chooses between burning glucose and fatty acids for energy. Enzymes and hormones play a key role…
11 Amazing Tips to Improve Your Sleep Quality
Limit Power NapsModulate Sunlight ExposurePay Attention to CaffeineSchedule BedtimePlan Ahead for DinnertimeMelatonin: Not what you thoughtSleep EnvironmentHot Bath or ShowerEliminate Blue LightSleep StackAdrenal CocktailMagnesium The…
Gout: Symptoms & Natural Treatment
Osteoarthritis Symptoms & Home Remedies
Key Takeaways Lifestyle adjustments and alternative therapies contribute to overall symptom management. Low-impact exercises and physical activity help maintain mobility and reduce pain. Heat and…
The EWG Dirty Dozen: What You Need to Know
Key Takeaways The Dirty Dozen list highlights fruits and vegetables with the highest levels of pesticide residues. In 2024, strawberries, spinach, and kale top the…
Does Grounding or Earthing Actually Work?
Melatonin: Functions and Benefits
Key Takeaways Melatonin helps regulate sleep-wake cycles, signaling the body to rest as it gets dark. It acts as an antioxidant, protecting cells from damage….
Ceruloplasmin: The Master Antioxidant
Key Takeaways: Ceruloplasmin is a copper-containing enzyme essential for iron metabolism and preventing oxidative stress. It helps transport iron safely, preventing iron overload in tissues…
Elimination Diets: Find the Foods Behind Your Symptoms
Key Takeaways Elimination diets identify food intolerances by removing and reintroducing specific foods. Divided into two phases: elimination and reintroduction. Items like gluten, soy, and…
Gestational Diabetes Management: Expert Tips for Success
Key Highlights Gestational diabetes, marked by glucose intolerance during pregnancy, requires careful blood sugar control. A healthy pregnancy with gestational diabetes includes regular exercise, a…
GABA (gamma-aminobutyric acid)
How Insulin Regulates Blood Sugar
Key Takeaways Insulin helps regulate blood sugar by moving glucose into cells. Imbalances in insulin levels can cause conditions like diabetes. Insulin resistance can lead…
Are Energy Drinks Dangerous?
Key Takeaways: Caffeine is the most common stimulant in energy drinks. Sugar, though harmful, is widely used in energy drinks. Electrolytes help maintain hydration and…
Oxidative Stress: Causes, Effects, Solutions
Key Takeaways Oxidative stress results from an imbalance between free radicals and antioxidants in the body, leading to cellular damage. Chronic oxidative stress contributes to…
Do Artificial Sweeteners Cause Weight Gain? The Surprising Truth
Key Takeaways – Artificial sweeteners may disrupt gut microbiome balance, impacting digestion and immune health. – These sweeteners can interfere with natural metabolism, leading to…
Superoxide Dismutase: Your Body’s Antioxidant Defender
Key Takeaways SOD protects against oxidative stress by neutralizing free radicals. Copper is necessary for SOD to function. Low SOD activity can lead to aging,…
What You Need to Know About Salt and Your Health
Table of ContentsThe Health Benefits of Unrefined Sea SaltElectrolyte BalanceMineral ContentImproved HydrationBoosted Energy LevelsImmune SupportImproved…
Minimalist Travel: Less Baggage, More Memories
Key Takeaways Learn to pack only essential items for any trip, keeping your luggage light….
Vitamin K2 and The Calcium Paradox by Kate Rheaume-Bleue
Key Takeaways Explains Vitamin K2’s role in calcium distribution. Links deficiency to bone and heart…
Metabolic Syndrome: Managing This Health Risk
Key Takeaways Metabolic syndrome is a cluster of conditions increasing the risk of heart disease,…
7 Physical Benefits of Gardening: Green Thumb, Healthy Heart
Key Highlights Gardening activities such as landscaping, planting, and maintaining plants can help reduce blood…
Triglycerides: Levels & Range Explained
Key Highlights Triglycerides are the most common form of fat in the body play a…
Breast Milk or Formula: Which Is Healthier for Your Baby?
Key Highlights Breast milk is ideal for infants, offering essential nutrients, cognitive development support, and…
Vegetable Oil: Health Risks You Might Not Know
Key Takeaways: Omega-6 fats from vegetable oils cause oxidative stress and inflammation. Reducing omega-6 intake…
The Bulletproof Diet by Dave Asprey
The Bulletproof Diet is a nutrition and lifestyle book authored by Dave Asprey, the founder…
Brain Energy by Dr. Christopher Palmer
Key Takeaways Connects mental health with metabolic health. Proposes ketogenic diet for brain disorders. Discusses…
9 Vital Travel Tips for Pregnant Women
Key Takeaways Consult Your Doctor: Always discuss travel plans with your healthcare provider to ensure…