Key Takeaways
- Inflammation is the body’s response to injury or infection, but chronic inflammation can lead to health problems.
- Iron overload from artificial sources and copper deficiency contribute to chronic inflammation.
- Acute inflammation is temporary and protective, while chronic inflammation can cause long-term damage.
- Managing inflammation involves dietary choices, avoiding fortified foods, and ensuring sufficient copper intake.
- Animal-based foods are vital for reducing inflammation and maintaining nutrient balance.
What is Inflammation?
Inflammation is the body’s response to injury, infection, or harmful stimuli. It presents as redness, heat, swelling, and pain.
Acute inflammation is a short-term reaction that aids in healing and defense. Chronic inflammation, however, can lead to tissue damage and contribute to diseases like heart disease and diabetes.
Causes of Inflammation
Inflammation can be triggered by various factors, depending on whether it is acute or chronic.
Acute Inflammation
This type occurs quickly after injury or infection and usually resolves once the threat is eliminated. Common triggers include injuries, bacterial or viral infections, and exposure to irritants.
Chronic Inflammation
Chronic inflammation develops over time and can persist for months or years. Dietary factors, such as consuming processed foods fortified with iron, can lead to iron overload, which contributes to oxidative stress and chronic inflammation.
Copper deficiency also plays a role in chronic inflammation, as copper is essential for regulating iron metabolism and reducing oxidative stress.
Symptoms of Inflammation

Symptoms vary depending on whether inflammation is acute or chronic.
Acute Inflammation Symptoms
Symptoms include redness, swelling, pain, and heat at the affected site. These are signs that the body is working to repair damage or fight off infection.
Chronic Inflammation Symptoms
Chronic inflammation symptoms are often subtle and may include fatigue, joint pain, digestive issues, and unexplained aches.
These symptoms can be exacerbated by factors like iron overload and copper deficiency.
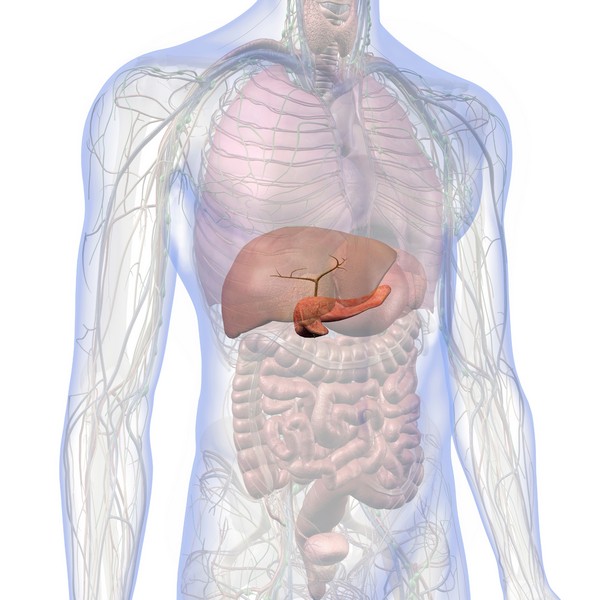
Impact of Inflammation on Health
While inflammation is protective in the short term, it can lead to serious health problems if it becomes chronic.
Short-Term vs. Long-Term Effects
Acute inflammation helps in healing and protection against infections. However, prolonged inflammation can contribute to chronic diseases, including cardiovascular diseases, autoimmune disorders, and metabolic conditions.
Iron overload from artificial sources, such as supplements and fortified foods, can worsen these conditions by increasing oxidative stress.
Copper deficiency can impair the body’s ability to manage inflammation, leading to further health complications.
Dietary Influence on Inflammation

Diet plays a major role in either promoting or reducing inflammation.
Pro-Inflammatory Foods to Avoid
Avoiding ultra-processed foods that are fortified with iron is important in managing inflammation. These foods can lead to iron overload, which contributes to chronic inflammation.
It’s also beneficial to reduce intake of sugar, refined carbohydrates, and vegetable oils, which can promote inflammation.
Anti-Inflammatory Foods to Include
Eat bioavailable whole foods that are naturally rich in nutrients. Foods like grass-fed beef, pastured eggs, and cod liver oil provide essential fatty acids and vitamins that help reduce inflammation.
Including copper-rich foods such as liver and shellfish helps maintain the necessary balance between iron and copper, preventing deficiencies that can exacerbate inflammation.
Iron Overload and Copper Deficiency
Understanding the roles of iron and copper in the body is key to managing inflammation.
Understanding Iron Overload
Iron overload, particularly from artificial sources like fortified foods and supplements, contributes to oxidative stress and chronic inflammation.
Unlike iron obtained from natural food sources like red meat, artificial iron can accumulate in the body and cause harm.
This condition, often exacerbated by genetic factors like hemochromatosis, can lead to severe health problems if left unmanaged.
The Role of Copper Deficiency
Copper is essential for reducing inflammation and regulating iron levels. A deficiency in copper can lead to increased oxidative stress, impaired immune function, and difficulty managing iron levels, all of which contribute to chronic inflammation.
Ensuring adequate copper intake through diet is vital for maintaining health and preventing inflammation.
Lifestyle Factors Affecting Inflammation

Several lifestyle factors play a role in managing inflammation.
Physical Activity
Regular physical activity helps reduce inflammation by improving circulation and reducing stress.
Exercise can also help regulate the immune system and maintain a healthy weight, both of which are important in managing inflammation.
Stress Management
Chronic stress is a significant contributor to inflammation. Managing stress through techniques like meditation, deep breathing, and adequate sleep can help reduce inflammatory responses in the body.
Environmental Toxins
Exposure to environmental toxins, such as pollutants, chemicals, and heavy metals, can increase inflammation.
Reducing exposure to these toxins by choosing natural cleaning products, avoiding processed foods, and filtering water can help manage inflammation.
Natural Remedies

Natural remedies and supplements can be effective in managing inflammation.
Cod Liver Oil
Cod liver oil is rich in omega-3 fatty acids and vitamins A and D, which are known for their anti-inflammatory properties.
Including cod liver oil in your diet can help reduce inflammation and support overall health.
Herbal Supplements
Herbs like turmeric and ginger have strong anti-inflammatory properties and can be effective in reducing chronic inflammation.
These natural supplements can be incorporated into the diet through teas, extracts, or culinary use.
Managing Iron and Copper Levels
Balancing iron and copper intake is important for managing inflammation. Avoiding fortified foods and unnecessary iron supplements helps prevent iron overload, while consuming copper-rich foods ensures that iron levels remain in check.
Copper supplementation may be necessary to restore balance and reduce inflammation.
Conclusion
Chronic inflammation poses significant health risks, but it can be managed through dietary choices, lifestyle changes, and natural remedies. Avoiding artificial sources of iron, ensuring adequate copper intake, and focusing on nutrient-dense animal-based foods helps reduce inflammation and support overall health.
FAQ
How does iron overload contribute to inflammation?
Iron overload, particularly from artificial sources like fortified processed foods and supplements, increases oxidative stress, leading to chronic inflammation and associated health problems.
What are the signs of copper deficiency?
Signs include fatigue, weakened immune function, and difficulty regulating iron levels. Copper deficiency can also contribute to chronic inflammation.
Can dietary changes help manage iron overload?
Yes, avoiding artificially fortified foods and iron supplements, and instead obtaining iron from natural food sources like red meat, can help manage iron overload.
How do I balance iron and copper in my diet?
Include copper-rich foods like liver and shellfish, and be mindful of your iron intake, avoiding artificial sources to prevent overload.
What lifestyle changes can reduce inflammation?
Regular physical activity, stress management, and minimizing exposure to environmental toxins are key strategies to reduce inflammation.
Research
Batey RG, Lai Chung Fong P, Shamir S, Sherlock S. A non-transferrin-bound serum iron in idiopathic hemochromatosis. Dig Dis Sci. 1980 May;25(5):340-6. doi: 10.1007/BF01308057. PMID: 7371472.
Bo, S., Durazzo, M., Gambino, R., Berutti, C., Milanesio, N., Caropreso, A., Gentile, L., Cassader, M., Cavallo-Perin, P. and Pagano, G., 2008. Associations of Dietary and Serum Copper with Inflammation, Oxidative Stress, and Metabolic Variables in Adults ,. The Journal of Nutrition, [online] 138(2), pp.305–310. https://doi.org/10.1093/jn/138.2.305.
Boddaert, N., Le Quan Sang, K. H., Rötig, A., Leroy-Willig, A., Gallet, S., Brunelle, F., Sidi, D., Thalabard, J., Munnich, A., & Cabantchik, Z. I. (2007). Selective iron chelation in Friedreich ataxia: Biologic and clinical implications. Blood, 110(1), 401-408. https://doi.org/10.1182/blood-2006-12-065433
Collins, J. F. (2021). Copper nutrition and biochemistry and human (patho)physiology. Advances in Food and Nutrition Research, 96, 311-364. https://doi.org/10.1016/bs.afnr.2021.01.005
Cornelissen, A., Guo, L., Sakamoto, A., Virmani, R. and Finn, A.V., 2019. New insights into the role of iron in inflammation and atherosclerosis. EBioMedicine, [online] 47, pp.598–606.
https://doi.org/10.1016/j.ebiom.2019.08.014.
DiNicolantonio, J.J., Mangan, D. and O’Keefe, J.H., 2018. The fructose–copper connection: Added sugars induce fatty liver and insulin resistance via copper deficiency. Journal of Metabolic Health, [online] 3(1).
https://doi.org/10.4102/jir.v3i1.43.
Fillebeen, C., Descamps, L., Dehouck, M.-P., Fenart, L., Benaïssa, M., Spik, G., Cecchelli, R. and Pierce, A., 1999. Receptor-mediated Transcytosis of Lactoferrin through the Blood-Brain Barrier. Journal of Biological Chemistry, [online] 274(11), pp.7011–7017. https://doi.org/10.1074/jbc.274.11.7011.
Gaetke, L., 2003. Copper toxicity, oxidative stress, and antioxidant nutrients. Toxicology, [online] 189(1–2), pp.147–163. https://doi.org/10.1016/s0300-483x(03)00159-8.
Galaris, D., Barbouti, A. and Pantopoulos, K., 2019. Iron homeostasis and oxidative stress: An intimate relationship. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research, [online] 1866(12), p.118535. https://doi.org/10.1016/j.bbamcr.2019.118535.
Greenberg, G.R. and Wintrobe, M.M., 1946. A LABILE IRON POOL. Journal of Biological Chemistry, [online] 165(1), pp.397–398. https://doi.org/10.1016/s0021-9258(17)41250-6.
Gutteridge, J.M.C. and Halliwell, B., 2018. Mini-Review: Oxidative stress, redox stress or redox success? Biochemical and Biophysical Research Communications, [online] 502(2), pp.183–186.
https://doi.org/10.1016/j.bbrc.2018.05.045.
Harris, Z. L., Durley, A. P., Man, T. K., & Gitlin, J. D. (1999). Targeted gene disruption reveals an essential role for ceruloplasmin in cellular iron efflux. Proceedings of the National Academy of Sciences of the United States of America, 96(19), 10812-10817. https://doi.org/10.1073/pnas.96.19.10812
Hentze, M.W., Muckenthaler, M.U., Galy, B. and Camaschella, C., 2010. Two to Tango: Regulation of Mammalian Iron Metabolism. Cell, [online] 142(1), pp.24–38. https://doi.org/10.1016/j.cell.2010.06.028.
Ke, Y. and Qian, Z.M., 2007. Brain iron metabolism: Neurobiology and neurochemistry. Progress in Neurobiology, [online] 83(3), pp.149–173. https://doi.org/10.1016/j.pneurobio.2007.07.009.
Kenkhuis, B., Bush, A.I. and Ayton, S., 2023. How iron can drive neurodegeneration. Trends in Neurosciences, [online] 46(5), pp.333–335.
https://doi.org/10.1016/j.tins.2023.02.003.
Kruszewski, M., 2003. Labile iron pool: the main determinant of cellular response to oxidative stress. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis, [online] 531(1–2), pp.81–92.
https://doi.org/10.1016/j.mrfmmm.2003.08.004.
Milanino, R., Conforti, A., Franco, L., Marrella, M. and Velo, G., 1985. Review: Copper and inflammation — a possible rationale for the pharmalogical manipulation of inflammatory discorders. Agents and Actions, [online] 16(6), pp.504–513. https://doi.org/10.1007/bf01983655.
Mills, E., Dong, X., Wang, F. and Xu, H., 2009. Mechanisms of Brain Iron Transport: Insight into Neurodegeneration and CNS Disorders. Future Medicinal Chemistry, [online] 2(1), pp.51–64. https://doi.org/10.4155/fmc.09.140.
Moos T., Morgan EH. Transferrin and transferrin receptor function in brain barrier systems. Cell Mol Neurobiol. 2000 Feb;20(1):77-95. doi: 10.1023/a:1006948027674. PMID: 10690503.
Moos, T., Nielsen, T.R., Skjørringe, T. and Morgan, E.H., 2007. Iron trafficking inside the brain. Journal of Neurochemistry, [online] 103(5), pp.1730–1740. https://doi.org/10.1111/j.1471-4159.2007.04976.x.
Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197-213. doi: 10.1146/annurev.nutr.28.061807.155521. PMID: 18489257.
Prohaska, J. R. (2011). Impact of Copper Limitation on Expression and Function of Multicopper Oxidases (Ferroxidases). Advances in Nutrition, 2(2), 89-95. https://doi.org/10.3945/an.110.000208
Sorenson, J.R.J., 1989. 6 Copper Complexes Offer a Physiological Approach to Treatment of Chronic Diseases. Progress in Medicinal Chemistry, [online] pp.437–568. https://doi.org/10.1016/s0079-6468(08)70246-7.
Thackeray EW, Sanderson SO, Fox JC, Kumar N. Hepatic iron overload or cirrhosis may occur in acquired copper deficiency and is likely mediated by hypoceruloplasminemia. J Clin Gastroenterol. 2011 Feb;45(2):153-8. doi: 10.1097/MCG.0b013e3181dc25f7. PMID: 20502350.
Uriu-Adams, J.Y. and Keen, C.L., 2005. Copper, oxidative stress, and human health. Molecular Aspects of Medicine, [online] 26(4–5), pp.268–298. https://doi.org/10.1016/j.mam.2005.07.015.
Vashchenko, G., & A. MacGillivray, R. T. (2013). Multi-Copper Oxidases and Human Iron Metabolism. Nutrients, 5(7), 2289-2313. https://doi.org/10.3390/nu5072289
Wang, J. and Pantopoulos, K., 2011. Regulation of cellular iron metabolism. Biochemical Journal, [online] 434(3), pp.365–381. https://doi.org/10.1042/bj20101825.
Wallander, M.L., Leibold, E.A. and Eisenstein, R.S., 2006. Molecular control of vertebrate iron homeostasis by iron regulatory proteins. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research, [online] 1763(7), pp.668–689. https://doi.org/10.1016/j.bbamcr.2006.05.004.
Ward, R.J., Zucca, F.A., Duyn, J.H., Crichton, R.R. and Zecca, L., 2014. The role of iron in brain ageing and neurodegenerative disorders. The Lancet Neurology, [online] 13(10), pp.1045–1060.
https://doi.org/10.1016/s1474-4422(14)70117-6.
Xia, Y., Chen, Z., Huang, C., Shi, L., Ma, W., Chen, X., Liu, Y., Wang, Y., Cai, C., Huang, Y., Liu, W., Shi, R. and Luo, Q., 2024. Investigation the mechanism of iron overload-induced colonic inflammation following ferric citrate exposure. Ecotoxicology and Environmental Safety, [online] 275, p.116241. https://doi.org/10.1016/j.ecoenv.2024.116241.
Supporting Mental Health with Gut Health
Key Takeaways Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis. Probiotics: Beneficial bacteria that help regulate mood and support…
Iron Overload: Symptoms & Prevention Tips
Key Takeaways: Iron overload happens when the body absorbs excessive iron, which can damage organs. Common symptoms include fatigue, joint pain, and skin changes. Early…
Diabetes: Everything You Need to Know
Atherosclerosis Prevention Strategies: Insights from Scientific Research
Key Takeaways Atherosclerosis is the hardening and narrowing of arteries caused by plaque buildup. Chronic inflammation and oxidative stress contribute to the development of plaque….
7 Remedies for Kidney Stones: A Comprehensive Guide
Key Takeaways Staying well-hydrated and adopting a balanced diet can help prevent kidney stones. Knowing the causes of kidney stones can inform effective prevention strategies….
Alzheimer’s Disease: Symptoms, Causes, Treatment
Key Takeaways Alzheimer’s disease is a progressive neurodegenerative disorder affecting memory, thinking, and behavior. Oxidative stress, including from excess iron, plays a significant role in…
Triglycerides: Levels & Range Explained
Key Highlights Triglycerides are the most common form of fat in the body play a role in energy storage High levels of triglycerides can increase…
Proteolytic Enzymes and Heart Health: What the Research Shows
Your heart works tirelessly to pump blood throughout your body, delivering essential nutrients and oxygen to your cells. However, factors like poor diet, stress, and…
L-Glutamine and Gut Health: Benefits and Side Effects
Key Takeaways L-Glutamine is essential for gut health. Benefits include improved digestion and reduced inflammation. Potential side effects are rare but can occur in high…
Uric Acid: Effects & Management
Key Takeaways Uric acid plays a central role in metabolic health and oxidative stress regulation. Elevated uric acid levels are linked to gout, metabolic syndrome,…
Alcohol and Its Effects
Key Takeaways Alcohol is metabolized primarily in the liver, producing acetaldehyde, a toxic byproduct. Chronic alcohol consumption leads to liver damage, including fatty liver, hepatitis,…
Metabolic Health: What It Means and How to Improve It
Key Takeaways Metabolic health reflects how well your body processes energy and maintains stable blood sugar, cholesterol, and blood pressure. Key indicators of metabolic health…
Postbiotics: What They Are and Why They Are Important
Key Takeaways Postbiotics 101: They’re beneficial by-products from probiotics that consume prebiotics Boosts Immunity: Postbiotics sharpen your immune system, helping fight off pathogens and reducing…
SIBO Bloating: Causes, Diet, & Management Tips
Key Takeaways SIBO disrupts gut bacteria balance, causing bloating, pain, and nutrient absorption issues. Symptoms include bloating, abdominal pain, diarrhea, constipation, weight loss, and fatigue….
Histamine: What You Should Know
Key Takeaways Histamine’s Role: Vital in immune responses, digestion, and as a neurotransmitter in the central nervous system. Histamine Production: Produced in mast cells and…
Inflammation: Causes & Effects
Key Takeaways Inflammation is the body’s response to injury or infection, but chronic inflammation can lead to health problems. Iron overload from artificial sources and…
Chronic Kidney Disease (CKD): Causes & Treatment
Key Takeaways Ultra-processed foods and high carbohydrate intake worsen inflammation, harming kidney function. Iron overload leads to oxidative stress, which accelerates CKD progression. Copper is…
Insulin Resistance: What It Is & How to Manage It
Key Takeaways Insulin resistance leads to high blood sugar when cells stop responding to insulin. Often connected to obesity, poor diet, and physical inactivity. Symptoms…
Signs of Diabetes: Recognizing the Red Flags
Key Takeaways Increased Thirst and Urination: High blood sugar leads to dehydration, causing excessive thirst and frequent urination. Unexplained Weight Loss: Diabetes can cause the…
Coping with Pet Allergies: Tips & Advice
Key Highlights Pet allergies often cause sneezing, coughing, itchy eyes, and skin rash. Pet allergens are in the saliva, urine, and dander of furry animals….
Dialysis: Benefits & Challenges
Key Takeaways Dialysis removes waste and excess fluid from the blood when kidneys cannot function. Two main types: hemodialysis (machine-based) and peritoneal dialysis (abdomen-based). Dialysis…
Travel Hygiene Tips: Stay Fresh on the Go
Key Highlights Key practices include frequent handwashing, showering, and oral care. Packing a portable hygiene kit can help you stay fresh on the go. Advanced…
Is Eating Sugar Really That Bad For Your Health?
Should You Really Be Concerned? In short, YES! Thank you, that’s all folks, and do have a good evening. Seriously though, extensive research has established…
7 Simple Tips for Lowering Blood Pressure Naturally
Maintaining healthy blood pressure levels is essential for overall well-being, as high blood pressure can lead to serious health complications. However, it is possible to…
Allergy-Friendly Pets
Key Highlights Hypoallergenic pets are great for people with pet allergies, as they produce fewer allergens like dander, saliva, and proteins that can trigger symptoms….
How to Lower Triglycerides Fast: Natural Solutions
Key Highlights Triglycerides, a type of fat found in the blood, are essential indicators of metabolic health. Elevated triglyceride levels increase the risk of heart…
Quit Sugar for 14 Days: What Happens to Your Body?
Key Takeaways: Immediate Health Benefits of Reducing Sugar: In just two weeks, enjoy enhanced energy levels, weight loss, a reduced risk of chronic diseases, and…
High Homocysteine: How to Manage Levels
Key Takeaways: Elevated homocysteine can raise the risk of heart disease and other health problems. Animal-based foods high in B vitamins help reduce homocysteine levels….
Parkinson’s Disease : Symptoms, Causes & Treatment
Key Takeaways Parkinson’s disease is a progressive neurological disorder that affects movement and coordination. Oxidative stress and excess iron are significant factors in the progression…
Remnant Cholesterol (RC): Its Origins & Impact
Key Takeaways Remnant cholesterol (RC) is the cholesterol content left in the blood after triglycerides are removed from VLDL and IDL particles. RC is a…
Vegetable Oil: Health Risks You Might Not Know
Key Takeaways: Omega-6 fats from vegetable oils cause oxidative stress and inflammation. Reducing omega-6 intake and using stable fats can lower health risks. High triglycerides…
Boost Insulin Sensitivity Naturally
Key Takeaways Improving insulin sensitivity helps control blood sugar and reduces the risk of metabolic disorders. Regular physical activity enhances how cells respond to insulin….
Metabolic Syndrome: Managing This Health Risk
Key Takeaways Metabolic syndrome is a cluster of conditions increasing the risk of heart disease, stroke, and diabetes. Symptoms include high blood pressure, high blood…
Non-Alcoholic Fatty Liver Disease (NAFLD)
Key Takeaways NAFLD involves fat buildup in the liver not caused by alcohol. Commonly associated with obesity, insulin resistance, and metabolic syndrome. NAFLD can lead…