Key Takeaways
Uric acid plays a central role in metabolic health and oxidative stress regulation.
Elevated uric acid levels are linked to gout, metabolic syndrome, and cardiovascular diseases.
High fructose consumption is a major factor in uric acid overproduction and fat accumulation.
Copper deficiency and iron dysregulation contribute to oxidative stress, impacting uric acid metabolism.
Natural animal-based diets, including red meat, provide essential nutrients that regulate uric acid.
Introduction

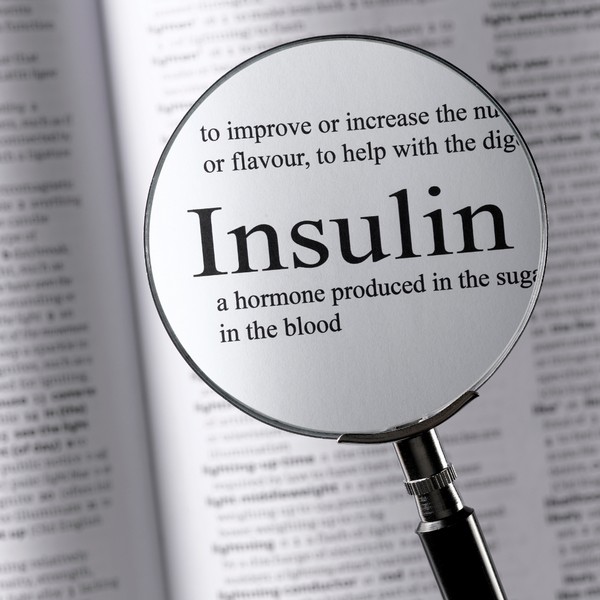
Uric acid is a compound produced during the breakdown of purines, which are found in many foods and naturally occurring in the body.
While uric acid serves important antioxidant functions, excess levels can lead to health conditions such as gout and kidney stones.
Uric Acid Metabolism
Purine Breakdown and Uric Acid Production
Purines are substances found in both food and body tissues. When purines break down, uric acid is produced.
Most uric acid dissolves in the blood and is excreted by the kidneys. Problems arise when the body either produces too much uric acid or fails to excrete enough, leading to elevated serum uric acid levels.
Factors Influencing Uric Acid Levels
Several factors can influence uric acid levels in the body, including diet, kidney function, and metabolic processes.
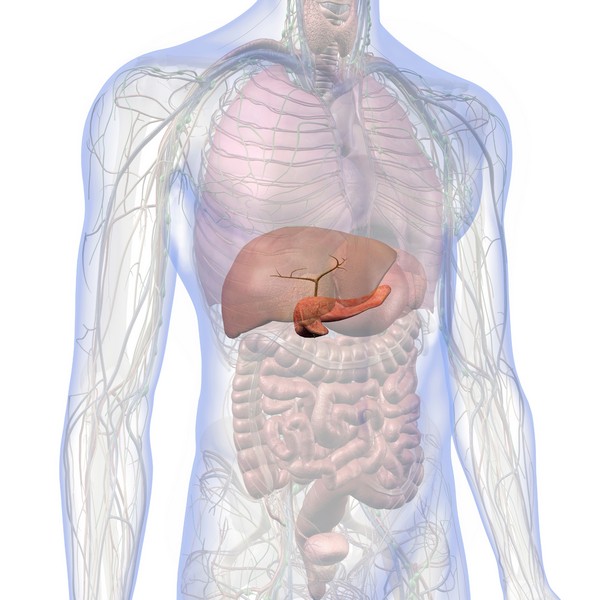
High consumption of fructose is a key contributor to increased uric acid production. This occurs because fructose metabolism generates a large amount of uric acid, particularly in the liver.
Uric Acid and Fructose

Fructose, found in sugary beverages and high-fructose corn syrup, is metabolized differently than other sugars.
Unlike glucose, fructose undergoes rapid metabolism in the liver, leading to the depletion of ATP (the body’s energy currency) and the production of uric acid.
This process contributes to metabolic syndrome, fatty liver, and other health conditions. Reducing fructose intake is essential for lowering uric acid levels and improving metabolic health.
Iron Dysregulation and Oxidative Stress
The Role of Iron and Copper
Iron dysregulation, often exacerbated by copper deficiency, can lead to oxidative stress and metabolic disturbances.
Copper is critical in regulating iron and preventing its accumulation in tissues. When copper is deficient, iron builds up, leading to free radical damage and increased oxidative stress.
This oxidative stress further influences uric acid production and contributes to various health problems, including gout and cardiovascular disease.
Oxidative Stress and Uric Acid
Uric acid serves as an antioxidant in the bloodstream, but its overproduction, often triggered by factors like fructose consumption and iron dysregulation, can lead to harmful effects inside cells.
Intracellular uric acid promotes oxidative stress, inflammation, and fat accumulation, particularly in the liver.
This is a significant concern in metabolic disorders like non-alcoholic fatty liver disease (NAFLD).
Health Conditions Linked to Uric Acid

Gout
Gout is a painful condition caused by the accumulation of uric acid crystals in joints, leading to inflammation and discomfort.
While purine-rich foods are often blamed, the true drivers of elevated uric acid in gout are metabolic factors like fructose consumption, oxidative stress, and kidney function.
Addressing these underlying causes is key to managing gout effectively.
Metabolic Syndrome and NAFLD
Elevated uric acid levels are commonly seen in individuals with metabolic syndrome and non-alcoholic fatty liver disease (NAFLD).
These conditions are driven by insulin resistance, high carbohydrate intake, and fructose metabolism.
Lowering uric acid through dietary changes that reduce fructose and improve copper status can help mitigate these diseases.
Treatment and Management

Dietary Adjustments
Managing uric acid levels involves dietary changes focused on reducing fructose intake and optimizing nutrient balance.
Fructose, found in sugary drinks and processed foods, significantly contributes to uric acid overproduction.
Animal-based diets, particularly those rich in red meat, provide essential nutrients like copper and support metabolic health without contributing to uric acid-related problems.
Role of Medications
In some cases, medications like allopurinol are used to lower uric acid levels. These medications inhibit xanthine oxidase, an enzyme involved in uric acid production.
While effective, addressing the root causes through dietary and lifestyle changes is often the most sustainable approach.
Conclusion
Uric acid is a critical component of metabolic health, serving antioxidant functions in the body. However, when its levels become elevated due to factors like high fructose consumption, iron dysregulation, and oxidative stress, it can lead to conditions such as gout and metabolic syndrome. Prioritizing a nutrient-dense, animal-based diet and reducing fructose intake are essential strategies for managing uric acid levels and supporting overall health.
FAQs
What is the main cause of high uric acid levels?
Fructose consumption, not purine-rich foods, is a primary driver of high uric acid levels. It accelerates uric acid production during metabolism.
How does uric acid relate to gout?
Excess uric acid can form crystals in joints, leading to inflammation and gout. Managing fructose intake is key to reducing uric acid.
Does red meat cause high uric acid?
No. Red meat provides essential nutrients and does not significantly contribute to uric acid elevation. Carbohydrates and fructose are more likely culprits.
How can I lower my uric acid naturally?
Reduce fructose intake, optimize copper levels, and prioritize nutrient-dense foods like red meat to naturally lower uric acid levels.
What role does oxidative stress play in uric acid production?
Oxidative stress, often caused by iron dysregulation and fructose metabolism, increases uric acid production and contributes to metabolic diseases.
Research
Ayoub-Charette S, Liu Q, Khan TA, Au-Yeung F, Blanco Mejia S, de Souza RJ, Wolever TM, Leiter LA, Kendall C, Sievenpiper JL. Important food sources of fructose-containing sugars and incident gout: a systematic review and meta-analysis of prospective cohort studies. BMJ Open. 2019 May 5;9(5):e024171. doi: 10.1136/bmjopen-2018-024171. PMID: 31061018; PMCID: PMC6502023.
Bai, L., Zhou, J.-B., Zhou, T., Newson, R.B. and Cardoso, M.A., 2021. Incident gout and weight change patterns: a retrospective cohort study of US adults. Arthritis Research & Therapy, [online] 23(1). https://doi.org/10.1186/s13075-021-02461-7.
Basaranoglu, M., Basaranoglu, G., & Bugianesi, E. (2015). Carbohydrate intake and nonalcoholic fatty liver disease: Fructose as a weapon of mass destruction. Hepatobiliary Surgery and Nutrition, 4(2), 109-116. https://doi.org/10.3978/j.issn.2304-3881.2014.11.05
Cristina, M. (2023). Insulin and the kidneys: A contemporary view on the molecular basis. Frontiers in Nephrology, 3, 1133352.
https://doi.org/10.3389/fneph.2023.1133352
El Ridi, R., & Tallima, H. (2017). Physiological functions and pathogenic potential of uric acid: A review. Journal of Advanced Research, 8(5), 487-493. https://doi.org/10.1016/j.jare.2017.03.003
Ghio, A.J., Ford, E.S., Kennedy, T.P. and Hoidal, J.R., 2005. The association between serum ferritin and uric acid in humans. Free Radical Research, [online] 39(3), pp.337–342. https://doi.org/10.1080/10715760400026088.
Goldberg, E. L., Asher, J. L., Molony, R. D., Shaw, A. C., Zeiss, C. J., Wang, C., Morozova-Roche, L. A., Herzog, R. I., Iwasaki, A., & Dixit, V. D. (2017). β-hydroxybutyrate deactivates neutrophil NLRP3 inflammasome to relieve gout flares. Cell Reports, 18(9), 2077. https://doi.org/10.1016/j.celrep.2017.02.004
Jamnik, J., Rehman, S., Blanco Mejia, S., de Souza, R.J., Khan, T.A., Leiter, L.A., Wolever, T.M.S., Kendall, C.W.C., Jenkins, D.J.A. and Sievenpiper, J.L., 2016. Fructose intake and risk of gout and hyperuricemia: a systematic review and meta-analysis of prospective cohort studies. BMJ Open, [online] 6(10), p.e013191. https://doi.org/10.1136/bmjopen-2016-013191.
Kanbay, M., Segal, M., Afsar, B., Kang, D.-H., Rodriguez-Iturbe, B. and Johnson, R.J., 2013. The role of uric acid in the pathogenesis of human cardiovascular disease. Heart, [online] 99(11), pp.759–766. https://doi.org/10.1136/heartjnl-2012-302535.
Lanaspa, M.A., Sanchez-Lozada, L.G., Cicerchi, C., Li, N., Roncal-Jimenez, C.A., Ishimoto, T., Le, M., Garcia, G.E., Thomas, J.B., Rivard, C.J., Andres-Hernando, A., Hunter, B., Schreiner, G., Rodriguez-Iturbe, B., Sautin, Y.Y. and Johnson, R.J., 2012. Uric Acid Stimulates Fructokinase and Accelerates Fructose Metabolism in the Development of Fatty Liver. PLoS ONE, [online] 7(10), p.e47948. https://doi.org/10.1371/journal.pone.0047948.
Lanaspa, M.A., Tapia, E., Soto, V., Sautin, Y. and Sánchez-Lozada, L.G., 2011. Uric Acid and Fructose: Potential Biological Mechanisms. Seminars in Nephrology, [online] 31(5), pp.426–432. https://doi.org/10.1016/j.semnephrol.2011.08.006.
Maiuolo, J., Oppedisano, F., Gratteri, S., Muscoli, C. and Mollace, V., 2016. Regulation of uric acid metabolism and excretion. International Journal of Cardiology, [online] 213, pp.8–14. https://doi.org/10.1016/j.ijcard.2015.08.109.
Mainous, A.G., Knoll, M.E., Everett, C.J., Matheson, E.M., Hulihan, M.M. and Grant, A.M., 2011. Uric Acid as a Potential Cue to Screen for Iron Overload. The Journal of the American Board of Family Medicine, [online] 24(4), pp.415–421. https://doi.org/10.3122/jabfm.2011.04.110015.
Muscelli, E., 1996. Effect of insulin on renal sodium and uric acid handling in essential hypertension. American Journal of Hypertension, [online] 9(8), pp.746–752.
https://doi.org/10.1016/0895-7061(96)00098-2.
Nakagawa, T., Lanaspa, M. A., & Johnson, R. J. (2019). The effects of fruit consumption in patients with hyperuricaemia or gout. Rheumatology, 58(7), 1133-1141. https://doi.org/10.1093/rheumatology/kez128
Pina, A.F., Borges, D.O., Meneses, M.J., Branco, P., Birne, R., Vilasi, A. and Macedo, M.P., 2020. Insulin: Trigger and Target of Renal Functions. Frontiers in Cell and Developmental Biology, [online] 8.
https://doi.org/10.3389/fcell.2020.00519.
Rasool, M., Malik, A., Jabbar, U., Begum, I., Qazi, M.H., Asif, M., Naseer, M.I., Ansari, S.A., Jarullah, J., Haque, A. and Jamal, M.S., 2016. Effect of iron overload on renal functions and oxidative stress in beta thalassemia patients. Saudi Medical Journal, [online] 37(11), pp.1239–1242. https://doi.org/10.15537/smj.2016.11.16242.
Rho, Y.H., Zhu, Y. and Choi, H.K., 2011. The Epidemiology of Uric Acid and Fructose. Seminars in Nephrology, [online] 31(5), pp.410–419. https://doi.org/10.1016/j.semnephrol.2011.08.004.
Roman, Y. M. The Role of Uric Acid in Human Health: Insights from the Uricase Gene. Journal of Personalized Medicine, 13(9), 1409. https://doi.org/10.3390/jpm13091409
Singh, J.A., Reddy, S.G. and Kundukulam, J., 2011. Risk factors for gout and prevention: a systematic review of the literature. Current Opinion in Rheumatology, [online] 23(2), pp.192–202. https://doi.org/10.1097/bor.0b013e3283438e13.
Skøtt, P., Hother-Nielsen, O., Bruun, N.E., Giese, J., Nielsen, M.D., Beck-Nielsen, H. and Parving, H.-H., 1989. Effects of insulin on kidney function and sodium excretion in healthy subjects. Diabetologia, [online] 32(9). https://doi.org/10.1007/bf00274259.
So, A. and Thorens, B., 2010. Uric acid transport and disease. Journal of Clinical Investigation, [online] 120(6), pp.1791–1799. https://doi.org/10.1172/jci42344.
Wang, Y., Yang, Z., Wu, J., Xie, D., Yang, T., Li, H. and Xiong, Y., 2020. Associations of serum iron and ferritin with hyperuricemia and serum uric acid. Clinical Rheumatology, [online] 39(12), pp.3777–3785. https://doi.org/10.1007/s10067-020-05164-7.
Yamanaka H. [Alcohol ingestion and hyperuricemia]. Nihon Rinsho. 1996 Dec;54(12):3369-73. Japanese. PMID: 8976122.
Natural Remedies for Common Ailments: From Headaches to Allergies
Key Takeaways The appeal of natural remedies lies in their holistic approach, fewer side effects, and environmental sustainability. Specific natural remedies can effectively alleviate common…
Sunburn Prevention: Holistic and Natural Approaches
Key Takeaways A poor diet increases the risk of sunburn and skin damage. Short, regular sun exposure reduces the risk of sunburn. Early morning and…
The EWG Dirty Dozen: What You Need to Know
Key Takeaways The Dirty Dozen list highlights fruits and vegetables with the highest levels of pesticide residues. In 2024, strawberries, spinach, and kale top the…
Diatomaceous Earth: Natural Uses & Benefits
Key Takeaways – Diatomaceous earth is a natural powder made from fossilized algae called diatoms. – It helps cleanse the body of toxins and heavy…
DNA & Longevity: Can You Live to 200?
Key Takeaways: Longevity is shaped by a mix of genetics and lifestyle. Certain genes are linked to longer lifespans. Lifestyle choices can influence how long…
Managing Menopause Symptoms – A Guide to Navigate this Life Stage
Exercise RoutineManaging Stress Improving Sleep HabitsSeeking Emotional Support:Adjusting Your DietConsidering Alternative TherapiesFrequently Asked Questions Menopause is a natural stage in a woman’s life marking the…
Fluoride: Risks & Controversies
Key Takeaways Fluoride is widely used in dental products and water supplies, but its safety is debated. Overexposure to fluoride can lead to conditions like…
Osteoarthritis Symptoms & Home Remedies
Key Takeaways Lifestyle adjustments and alternative therapies contribute to overall symptom management. Low-impact exercises and physical activity help maintain mobility and reduce pain. Heat and…
Autism: Causes, Symptoms, and Management
Key Takeaways Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition that varies widely in symptoms and severity. Both genetic and environmental factors contribute to…
Elimination Diets: Find the Foods Behind Your Symptoms
Key Takeaways Elimination diets identify food intolerances by removing and reintroducing specific foods. Divided into two phases: elimination and reintroduction. Items like gluten, soy, and…
Oxidative Stress: Causes, Effects, Solutions
Key Takeaways Oxidative stress results from an imbalance between free radicals and antioxidants in the body, leading to cellular damage. Chronic oxidative stress contributes to…
The Randle Cycle: Glucose Fat Energy Dilemma
Key Takeaways The Randle Cycle explains how the body chooses between burning glucose and fatty acids for energy. Enzymes and hormones play a key role…
Superoxide Dismutase: Your Body’s Antioxidant Defender
Key Takeaways SOD protects against oxidative stress by neutralizing free radicals. Copper is necessary for SOD to function. Low SOD activity can lead to aging,…
How Insulin Regulates Blood Sugar
Do Artificial Sweeteners Cause Weight Gain? The Surprising Truth
Key Takeaways – Artificial sweeteners may disrupt gut microbiome balance, impacting digestion and immune health. – These sweeteners can interfere with natural metabolism, leading to…
Melatonin: Functions and Benefits
Key Takeaways Melatonin helps regulate sleep-wake cycles, signaling the body to rest as it gets dark. It acts as an antioxidant, protecting cells from damage….
Gestational Diabetes Management: Expert Tips for Success
Key Highlights Gestational diabetes, marked by glucose intolerance during pregnancy, requires careful blood sugar control. A healthy pregnancy with gestational diabetes includes regular exercise, a…
Adrenal Fatigue: Symptoms & Prevention
Key Takeaways: Adrenal fatigue is often linked to prolonged stress, leading to tiredness, brain fog, and mood swings. Disruptions in cortisol production can affect energy,…
Gout: Symptoms & Natural Treatment
Key Takeaways Gout results from the accumulation of uric acid crystals in the joints, causing severe pain and inflammation. High uric acid levels are often…
GABA (gamma-aminobutyric acid)
Why Sunlight is Essential for a Healthy Life
Key Takeaways Sunlight helps the body produce vitamin D, supporting bone health and immune function. Exposure to sunlight can improve mood and reduce symptoms of…
Are Energy Drinks Dangerous?
Key Takeaways: Caffeine is the most common stimulant in energy drinks. Sugar, though harmful, is widely used in energy drinks. Electrolytes help maintain hydration and…
Does Grounding or Earthing Actually Work?
Adrenal Cocktail: Recipe and Benefits
Key Takeaways The adrenal cocktail supports adrenal health and maintains energy levels. Combines potassium, sodium, and vitamin C for effective adrenal nourishment. Consumed in the…
11 Amazing Tips to Improve Your Sleep Quality
Limit Power NapsModulate Sunlight ExposurePay Attention to CaffeineSchedule BedtimePlan Ahead for DinnertimeMelatonin: Not what you thoughtSleep EnvironmentHot Bath or ShowerEliminate Blue LightSleep StackAdrenal CocktailMagnesium The…
Bromate: Its Impact on Your Thyroid & Nervous System
Key Takeaways Bromate is a toxic byproduct from water disinfection, impacting thyroid and nervous system health. It interferes with iodine, leading to thyroid dysfunction and…
Ceruloplasmin: The Master Antioxidant
Key Takeaways: Ceruloplasmin is a copper-containing enzyme essential for iron metabolism and preventing oxidative stress. It helps transport iron safely, preventing iron overload in tissues…
Trimethylglycine TMG: Betaine Anhydrous Explained
Key Takeaways Betaine Anhydrous (TMG) is a compound found naturally in various foods and offers…
5 Major Benefits of Omega-3 Fatty Acids
Key Takeaways Omega-3 fatty acids support heart health by reducing triglycerides and lowering blood pressure….
Inflammation: Causes & Effects
Key Takeaways Inflammation is the body’s response to injury or infection, but chronic inflammation can…
Breast Milk or Formula: Which Is Healthier for Your Baby?
Key Highlights Breast milk is ideal for infants, offering essential nutrients, cognitive development support, and…
Travel Hygiene Tips: Stay Fresh on the Go
Key Highlights Key practices include frequent handwashing, showering, and oral care. Packing a portable hygiene…
Allulose: The Best Sugar Alternative
Key Takeaways Allulose is a low-calorie sweetener found naturally in some fruits. It does not…
11 Amazing Tips to Improve Your Sleep Quality
Limit Power NapsModulate Sunlight ExposurePay Attention to CaffeineSchedule BedtimePlan Ahead for DinnertimeMelatonin: Not what you…
Vitamin K2 and The Calcium Paradox by Kate Rheaume-Bleue
Key Takeaways Explains Vitamin K2’s role in calcium distribution. Links deficiency to bone and heart…
Are Energy Drinks Dangerous?
Key Takeaways: Caffeine is the most common stimulant in energy drinks. Sugar, though harmful, is…
L-Carnitine: Benefits, Dosage, and Side Effects
Key Takeaways L-Carnitine supports fat metabolism and energy production. Benefits include enhanced exercise performance and…
Non-Alcoholic Fatty Liver Disease (NAFLD)
Key Takeaways NAFLD involves fat buildup in the liver not caused by alcohol. Commonly associated…