Key Takeaways:
- Ceruloplasmin is a copper-containing enzyme essential for iron metabolism and preventing oxidative stress.
- It helps transport iron safely, preventing iron overload in tissues and reducing the risk of damage.
- Low ceruloplasmin levels can increase oxidative damage and worsen inflammatory conditions.
- Adequate copper intake is vital for ceruloplasmin’s function and overall health.
- Ceruloplasmin is needed for protecting organs like the brain, liver, and kidneys.
What is Ceruloplasmin?
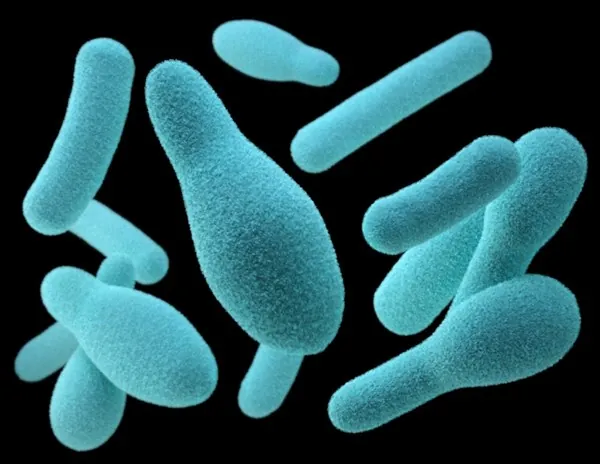
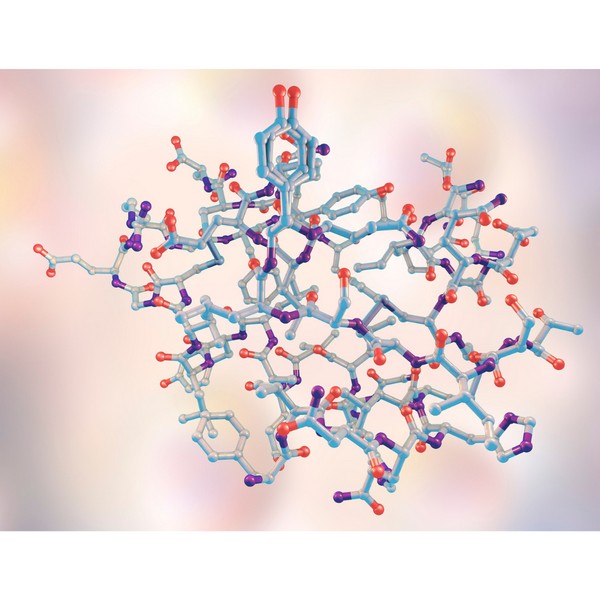
Ceruloplasmin is a copper-containing enzyme made in the liver and circulated in the blood. It regulates iron transport throughout the body. It contains six copper atoms per molecule, needed for its activity.
This enzyme also acts as an antioxidant, reducing oxidative stress by neutralizing free radicals, which helps maintain cellular health.
Deficiencies can lead to serious issues, including organ damage, inflammation, and neurodegenerative diseases. Maintaining healthy levels helps protect vital organs like the brain, liver, and kidneys.
Ceruloplasmin & Iron Metabolism
Regulating Iron Transport
One of ceruloplasmin’s key functions is managing iron by converting it into a transportable form (ferric iron).
This process lets iron bind to transferrin, a protein that safely moves iron through the bloodstream.
Without ceruloplasmin, free iron can build up in tissues, leading to overload, which can cause organ damage and inflammation.
Preventing Oxidative Stress
Ceruloplasmin helps limit oxidative stress by controlling free iron levels. Excess iron interacts with oxygen, producing harmful free radicals that damage cells.
Ceruloplasmin protects tissues, especially in the liver, kidneys, and brain, from oxidative damage by managing iron transport.
Ceruloplasmin & Copper Balance
Copper as a Co-factor
Ceruloplasmin’s function depends on copper. Copper activates ceruloplasmin and allows it to regulate iron.
Without enough copper, ceruloplasmin cannot manage iron levels effectively, leading to iron overload and oxidative damage.
Effects of Copper Deficiency on Ceruloplasmin Function
Copper deficiency can impair ceruloplasmin production and function. Low copper levels reduce ceruloplasmin, disrupting iron management.
This imbalance can lead to iron accumulation in organs, increasing oxidative stress and worsening chronic diseases like kidney disease and liver disorders.
Low Ceruloplasmin Health Conditions
Wilson’s Disease
Wilson’s disease is a genetic disorder where the body fails to eliminate excess copper. This condition is often connected to low ceruloplasmin levels, which causes copper buildup in the liver and brain, leading to organ damage.
Managing ceruloplasmin levels is key for preventing copper toxicity in people with Wilson’s disease.
Alzheimer’s and Neurodegenerative Diseases
Low ceruloplasmin levels have been linked to neurodegenerative diseases like Alzheimer’s.
Without enough ceruloplasmin, excess iron in the brain contributes to oxidative stress and harmful protein plaques. Balancing iron and reducing oxidative damage helps protect against cognitive decline.
Chronic Kidney Disease (CKD)
In CKD, low ceruloplasmin levels contribute to oxidative stress and inflammation, worsening the condition. Poor iron management increases the risk of kidney tissue damage.
Improving ceruloplasmin function through copper intake can help reduce these risks in CKD patients.
Diagnosing & Treating Ceruloplasmin Deficiency

Symptoms of Low Ceruloplasmin
Symptoms of low ceruloplasmin levels vary depending on the cause. Common signs include fatigue, anemia, neurological issues, and liver problems.
In severe cases, organ damage can occur due to unregulated iron or copper levels.
Testing for Ceruloplasmin Levels
Doctors can measure ceruloplasmin levels with a simple blood test. This test helps diagnose conditions such as Wilson’s disease, iron overload disorders, and assess copper and iron metabolism.
Treatment Strategies
Treatment for ceruloplasmin deficiency focuses on addressing the cause. Increasing copper intake through food or supplements can restore ceruloplasmin levels.
In cases like Wilson’s disease, medical interventions to reduce copper buildup are necessary. Managing iron intake may also help balance both copper and iron levels.
Supporting Ceruloplasmin Function Through Diet

Copper-Rich Foods
Eating foods rich in copper supports ceruloplasmin production. Great sources of copper include:
- Liver and organ meats
- Shellfish (e.g., oysters, crabs)
- Seeds and nuts (e.g., sunflower seeds, cashews)
- Dark chocolate
- Leafy greens like spinach
Nutrients That Support Ceruloplasmin Activity
Other nutrients help maintain a healthy balance of ceruloplasmin and iron. Zinc helps modulate copper levels, while vitamin C supports antioxidant function.
A balanced diet with these nutrients improves ceruloplasmin activity and protects against oxidative stress.
Conclusion
Ceruloplasmin is an enzyme that controls iron metabolism and protects the body from oxidative stress. Its functions depend on having enough copper, making proper copper intake important for preventing iron overload and organ damage. Managing ceruloplasmin levels helps reduce the risk of chronic conditions like Alzheimer’s and CKD.
FAQ Section
How does ceruloplasmin prevent iron overload?
Ceruloplasmin converts iron into a form that can be safely transported through the bloodstream, preventing iron buildup in tissues and reducing oxidative stress.
Why is copper important for ceruloplasmin function?
Copper activates ceruloplasmin, enabling it to regulate iron levels and protect tissues from oxidative damage caused by free iron.
What happens if ceruloplasmin levels are too low?
Low ceruloplasmin levels can lead to iron overload, increased oxidative stress, and organ damage, especially in the liver, brain, and kidneys.
Can a ceruloplasmin deficiency be treated with diet?
Yes, improving copper intake through copper-rich foods or supplements can help boost ceruloplasmin levels and restore iron balance in the body.
How is ceruloplasmin tested?
A simple blood test measures ceruloplasmin levels, often used to diagnose conditions like Wilson’s disease or assess copper and iron metabolism.
Research
Batey RG, Lai Chung Fong P, Shamir S, Sherlock S. A non-transferrin-bound serum iron in idiopathic hemochromatosis. Dig Dis Sci. 1980 May;25(5):340-6. doi: 10.1007/BF01308057. PMID: 7371472.
Bo, S., Durazzo, M., Gambino, R., Berutti, C., Milanesio, N., Caropreso, A., Gentile, L., Cassader, M., Cavallo-Perin, P. and Pagano, G., 2008. Associations of Dietary and Serum Copper with Inflammation, Oxidative Stress, and Metabolic Variables in Adults ,. The Journal of Nutrition, [online] 138(2), pp.305–310. https://doi.org/10.1093/jn/138.2.305.
Boddaert, N., Le Quan Sang, K. H., Rötig, A., Leroy-Willig, A., Gallet, S., Brunelle, F., Sidi, D., Thalabard, J., Munnich, A., & Cabantchik, Z. I. (2007). Selective iron chelation in Friedreich ataxia: Biologic and clinical implications. Blood, 110(1), 401-408. https://doi.org/10.1182/blood-2006-12-065433
Collins, J. F. (2021). Copper nutrition and biochemistry and human (patho)physiology. Advances in Food and Nutrition Research, 96, 311-364. https://doi.org/10.1016/bs.afnr.2021.01.005
DiNicolantonio, J.J., Mangan, D. and O’Keefe, J.H., 2018. The fructose–copper connection: Added sugars induce fatty liver and insulin resistance via copper deficiency. Journal of Metabolic Health, [online] 3(1).
https://doi.org/10.4102/jir.v3i1.43.
Fillebeen, C., Descamps, L., Dehouck, M.-P., Fenart, L., Benaïssa, M., Spik, G., Cecchelli, R. and Pierce, A., 1999. Receptor-mediated Transcytosis of Lactoferrin through the Blood-Brain Barrier. Journal of Biological Chemistry, [online] 274(11), pp.7011–7017. https://doi.org/10.1074/jbc.274.11.7011.
Gaetke, L., 2003. Copper toxicity, oxidative stress, and antioxidant nutrients. Toxicology, [online] 189(1–2), pp.147–163. https://doi.org/10.1016/s0300-483x(03)00159-8.
Galaris, D., Barbouti, A. and Pantopoulos, K., 2019. Iron homeostasis and oxidative stress: An intimate relationship. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research, [online] 1866(12), p.118535. https://doi.org/10.1016/j.bbamcr.2019.118535.
Greenberg, G.R. and Wintrobe, M.M., 1946. A LABILE IRON POOL. Journal of Biological Chemistry, [online] 165(1), pp.397–398. https://doi.org/10.1016/s0021-9258(17)41250-6.
Gutteridge, J.M.C. and Halliwell, B., 2018. Mini-Review: Oxidative stress, redox stress or redox success? Biochemical and Biophysical Research Communications, [online] 502(2), pp.183–186.
https://doi.org/10.1016/j.bbrc.2018.05.045.
Harris, Z. L., Durley, A. P., Man, T. K., & Gitlin, J. D. (1999). Targeted gene disruption reveals an essential role for ceruloplasmin in cellular iron efflux. Proceedings of the National Academy of Sciences of the United States of America, 96(19), 10812-10817. https://doi.org/10.1073/pnas.96.19.10812
Hentze, M.W., Muckenthaler, M.U., Galy, B. and Camaschella, C., 2010. Two to Tango: Regulation of Mammalian Iron Metabolism. Cell, [online] 142(1), pp.24–38. https://doi.org/10.1016/j.cell.2010.06.028.
Jeong, S.Y. and David, S., 2003. Glycosylphosphatidylinositol-anchored Ceruloplasmin Is Required for Iron Efflux from Cells in the Central Nervous System. Journal of Biological Chemistry, [online] 278(29), pp.27144–27148. https://doi.org/10.1074/jbc.m301988200.
Ke, Y. and Qian, Z.M., 2007. Brain iron metabolism: Neurobiology and neurochemistry. Progress in Neurobiology, [online] 83(3), pp.149–173. https://doi.org/10.1016/j.pneurobio.2007.07.009.
Kenkhuis, B., Bush, A.I. and Ayton, S., 2023. How iron can drive neurodegeneration. Trends in Neurosciences, [online] 46(5), pp.333–335.
https://doi.org/10.1016/j.tins.2023.02.003.
Kruszewski, M., 2003. Labile iron pool: the main determinant of cellular response to oxidative stress. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis, [online] 531(1–2), pp.81–92.
https://doi.org/10.1016/j.mrfmmm.2003.08.004.
Milanino, R., Conforti, A., Franco, L., Marrella, M. and Velo, G., 1985. Review: Copper and inflammation — a possible rationale for the pharmalogical manipulation of inflammatory discorders. Agents and Actions, [online] 16(6), pp.504–513. https://doi.org/10.1007/bf01983655.
Mills, E., Dong, X., Wang, F. and Xu, H., 2009. Mechanisms of Brain Iron Transport: Insight into Neurodegeneration and CNS Disorders. Future Medicinal Chemistry, [online] 2(1), pp.51–64. https://doi.org/10.4155/fmc.09.140.
Moos T., Morgan EH. Transferrin and transferrin receptor function in brain barrier systems. Cell Mol Neurobiol. 2000 Feb;20(1):77-95. doi: 10.1023/a:1006948027674. PMID: 10690503.
Moos, T., Nielsen, T.R., Skjørringe, T. and Morgan, E.H., 2007. Iron trafficking inside the brain. Journal of Neurochemistry, [online] 103(5), pp.1730–1740. https://doi.org/10.1111/j.1471-4159.2007.04976.x.
Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197-213. doi: 10.1146/annurev.nutr.28.061807.155521. PMID: 18489257.
Prohaska, J. R. (2011). Impact of Copper Limitation on Expression and Function of Multicopper Oxidases (Ferroxidases). Advances in Nutrition, 2(2), 89-95. https://doi.org/10.3945/an.110.000208
Sorenson, J.R.J., 1989. 6 Copper Complexes Offer a Physiological Approach to Treatment of Chronic Diseases. Progress in Medicinal Chemistry, [online] pp.437–568. https://doi.org/10.1016/s0079-6468(08)70246-7.
Uriu-Adams, J.Y. and Keen, C.L., 2005. Copper, oxidative stress, and human health. Molecular Aspects of Medicine, [online] 26(4–5), pp.268–298. https://doi.org/10.1016/j.mam.2005.07.015.
Vashchenko, G., & A. MacGillivray, R. T. (2013). Multi-Copper Oxidases and Human Iron Metabolism. Nutrients, 5(7), 2289-2313. https://doi.org/10.3390/nu5072289
Wang, J. and Pantopoulos, K., 2011. Regulation of cellular iron metabolism. Biochemical Journal, [online] 434(3), pp.365–381. https://doi.org/10.1042/bj20101825.
Wallander, M.L., Leibold, E.A. and Eisenstein, R.S., 2006. Molecular control of vertebrate iron homeostasis by iron regulatory proteins. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research, [online] 1763(7), pp.668–689. https://doi.org/10.1016/j.bbamcr.2006.05.004.
Ward, R.J., Zucca, F.A., Duyn, J.H., Crichton, R.R. and Zecca, L., 2014. The role of iron in brain ageing and neurodegenerative disorders. The Lancet Neurology, [online] 13(10), pp.1045–1060.
https://doi.org/10.1016/s1474-4422(14)70117-6.
Wang,J Kostas Pantopoulos; Regulation of cellular iron metabolism. Biochem J 15 March 2011; 434 (3): 365–381. doi: https://doi.org/10.1042/BJ20101825
Coping with Pet Allergies: Tips & Advice
Key Highlights Pet allergies often cause sneezing, coughing, itchy eyes, and skin rash. Pet allergens are in the saliva, urine, and dander of furry animals….
Alzheimer’s Disease: Symptoms, Causes, Treatment
Key Takeaways Alzheimer’s disease is a progressive neurodegenerative disorder affecting memory, thinking, and behavior. Oxidative stress, including from excess iron, plays a significant role in…
Supporting Mental Health with Gut Health
Key Takeaways Gut-Brain Connection: Gut health is directly linked to mental wellbeing through the gut-brain axis. Probiotics: Beneficial bacteria that help regulate mood and support…
Parkinson’s Disease : Symptoms, Causes & Treatment
Key Takeaways Parkinson’s disease is a progressive neurological disorder that affects movement and coordination. Oxidative stress and excess iron are significant factors in the progression…
Inflammation: Causes & Effects
Key Takeaways Inflammation is the body’s response to injury or infection, but chronic inflammation can lead to health problems. Iron overload from artificial sources and…
SIBO Bloating: Causes, Diet, & Management Tips
Key Takeaways SIBO disrupts gut bacteria balance, causing bloating, pain, and nutrient absorption issues. Symptoms include bloating, abdominal pain, diarrhea, constipation, weight loss, and fatigue….
Metabolic Health: What It Means and How to Improve It
Key Takeaways Metabolic health reflects how well your body processes energy and maintains stable blood sugar, cholesterol, and blood pressure. Key indicators of metabolic health…
Insulin Resistance: What It Is & How to Manage It
Key Takeaways Insulin resistance leads to high blood sugar when cells stop responding to insulin. Often connected to obesity, poor diet, and physical inactivity. Symptoms…
Is Eating Sugar Really That Bad For Your Health?
Should You Really Be Concerned? In short, YES! Thank you, that’s all folks, and do have a good evening. Seriously though, extensive research has established…
7 Simple Tips for Lowering Blood Pressure Naturally
Maintaining healthy blood pressure levels is essential for overall well-being, as high blood pressure can lead to serious health complications. However, it is possible to…
High Homocysteine: How to Manage Levels
Key Takeaways: Elevated homocysteine can raise the risk of heart disease and other health problems. Animal-based foods high in B vitamins help reduce homocysteine levels….
Triglycerides: Levels & Range Explained
Key Highlights Triglycerides are the most common form of fat in the body play a role in energy storage High levels of triglycerides can increase…
Remnant Cholesterol (RC): Its Origins & Impact
Key Takeaways Remnant cholesterol (RC) is the cholesterol content left in the blood after triglycerides are removed from VLDL and IDL particles. RC is a…
Allergy-Friendly Pets
Key Highlights Hypoallergenic pets are great for people with pet allergies, as they produce fewer allergens like dander, saliva, and proteins that can trigger symptoms….
Iron Overload: Symptoms & Prevention Tips
Key Takeaways: Iron overload happens when the body absorbs excessive iron, which can damage organs. Common symptoms include fatigue, joint pain, and skin changes. Early…
Uric Acid: Effects & Management
Key Takeaways Uric acid plays a central role in metabolic health and oxidative stress regulation. Elevated uric acid levels are linked to gout, metabolic syndrome,…
Postbiotics: What They Are and Why They Are Important
Key Takeaways Postbiotics 101: They’re beneficial by-products from probiotics that consume prebiotics Boosts Immunity: Postbiotics sharpen your immune system, helping fight off pathogens and reducing…
Atherosclerosis Prevention Strategies: Insights from Scientific Research
Key Takeaways Atherosclerosis is the hardening and narrowing of arteries caused by plaque buildup. Chronic inflammation and oxidative stress contribute to the development of plaque….
Vegetable Oil: Health Risks You Might Not Know
Key Takeaways: Omega-6 fats from vegetable oils cause oxidative stress and inflammation. Reducing omega-6 intake and using stable fats can lower health risks. High triglycerides…
Metabolic Syndrome: Managing This Health Risk
Key Takeaways Metabolic syndrome is a cluster of conditions increasing the risk of heart disease, stroke, and diabetes. Symptoms include high blood pressure, high blood…
Alcohol and Its Effects
Key Takeaways Alcohol is metabolized primarily in the liver, producing acetaldehyde, a toxic byproduct. Chronic alcohol consumption leads to liver damage, including fatty liver, hepatitis,…
Histamine: What You Should Know
Key Takeaways Histamine’s Role: Vital in immune responses, digestion, and as a neurotransmitter in the central nervous system. Histamine Production: Produced in mast cells and…
7 Remedies for Kidney Stones: A Comprehensive Guide
Key Takeaways Staying well-hydrated and adopting a balanced diet can help prevent kidney stones. Knowing the causes of kidney stones can inform effective prevention strategies….
Travel Hygiene Tips: Stay Fresh on the Go
Key Highlights Key practices include frequent handwashing, showering, and oral care. Packing a portable hygiene kit can help you stay fresh on the go. Advanced…
Chronic Kidney Disease (CKD): Causes & Treatment
Key Takeaways Ultra-processed foods and high carbohydrate intake worsen inflammation, harming kidney function. Iron overload leads to oxidative stress, which accelerates CKD progression. Copper is…
Proteolytic Enzymes and Heart Health: What the Research Shows
Your heart works tirelessly to pump blood throughout your body, delivering essential nutrients and oxygen to your cells. However, factors like poor diet, stress, and…
Non-Alcoholic Fatty Liver Disease (NAFLD)
Key Takeaways NAFLD involves fat buildup in the liver not caused by alcohol. Commonly associated with obesity, insulin resistance, and metabolic syndrome. NAFLD can lead…
Diabetes: Everything You Need to Know
Key Takeaways Type 1 and Type 2 diabetes involve insulin regulation issues, with Type 2 being the most common due to insulin resistance. Copper, retinol,…
Boost Insulin Sensitivity Naturally
Key Takeaways Improving insulin sensitivity helps control blood sugar and reduces the risk of metabolic disorders. Regular physical activity enhances how cells respond to insulin….
Dialysis: Benefits & Challenges
Key Takeaways Dialysis removes waste and excess fluid from the blood when kidneys cannot function. Two main types: hemodialysis (machine-based) and peritoneal dialysis (abdomen-based). Dialysis…
Quit Sugar for 14 Days: What Happens to Your Body?
Key Takeaways: Immediate Health Benefits of Reducing Sugar: In just two weeks, enjoy enhanced energy levels, weight loss, a reduced risk of chronic diseases, and…
Signs of Diabetes: Recognizing the Red Flags
Key Takeaways Increased Thirst and Urination: High blood sugar leads to dehydration, causing excessive thirst and frequent urination. Unexplained Weight Loss: Diabetes can cause the…
L-Glutamine and Gut Health: Benefits and Side Effects
Key Takeaways L-Glutamine is essential for gut health. Benefits include improved digestion and reduced inflammation. Potential side effects are rare but can occur in high…
How to Lower Triglycerides Fast: Natural Solutions
Key Highlights Triglycerides, a type of fat found in the blood, are essential indicators of metabolic health. Elevated triglyceride levels increase the risk of heart…
Lies I Taught in Medical School by Dr Robert Lufkin
Key Takeaways Metabolic dysfunction is a common cause of many chronic diseases. Conventional medical advice…
Benefits of Nutritional Yeast
Key Takeaways Nutritional yeast is a rich source of vitamins and minerals. It supports immune…
Adrenal Cocktail: Recipe and Benefits
Key Takeaways The adrenal cocktail supports adrenal health and maintains energy levels. Combines potassium, sodium,…
Anxiety: Causes, Symptoms, and Management
Key Takeaways: Anxiety can disrupt daily life when it becomes overwhelming. Common symptoms include restlessness,…
Dementia: Causes, Symptoms, and Management
Key Takeaways: Dementia involves a decline in cognitive function affecting memory, thinking, and daily life….
Mental Benefits of Learning a New Language
Key Takeaways: Enhances brain volume and memory. Improves cognitive flexibility, multitasking, and executive functions. Delays…
Increase GLP-1 Agonists Naturally
Key Takeaways: GLP-1 agonists regulate appetite, insulin production, and blood sugar levels. Regular exercise and…
Sustainable Beauty: Redefining Skincare with Eco-Friendly Practices
Key Highlights Sustainable beauty focuses on products that are good for the planet and consumer…
7 Key Hormones for Fat Burning
Key Takeaways: Hormones play a key role in regulating fat mobilization and utilization in the…
Potassium: Benefits & Sources
Key Takeaways Potassium is essential for regulating fluid balance, nerve signals, and muscle function. It…
13 Most Dangerous Foods Revealed
Key Highlights Fugu, or pufferfish, is one of the most poisonous foods in the world,…